Understanding B-cell lymphocytes
To understand CBCL you need to know a bit about your B-Cell lymphocytes.
B-Cell lymphocytes:
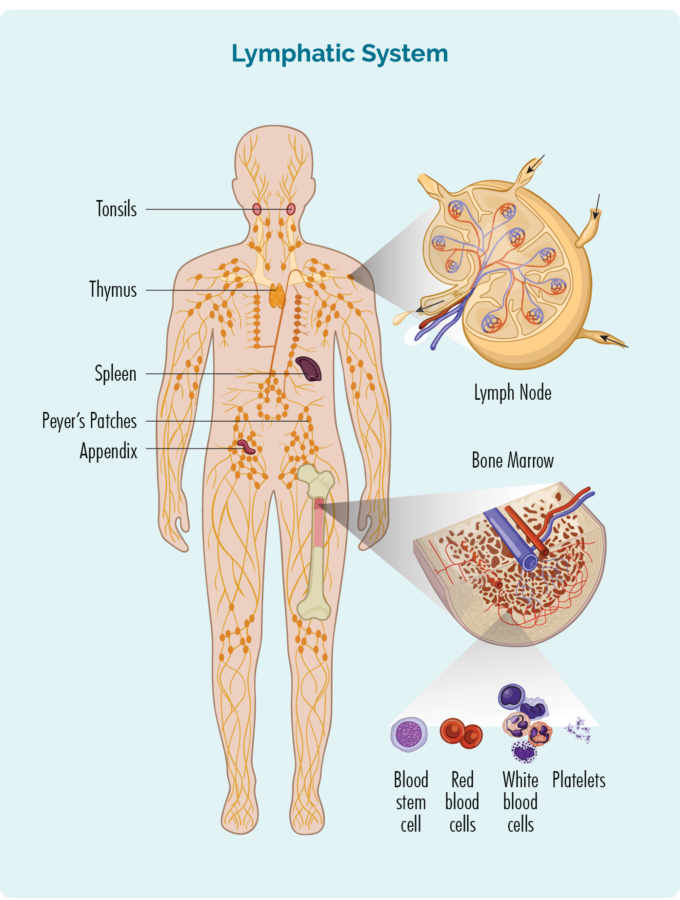
- Are a type of white blood cell.
- Fight infection and diseases to keep you healthy.
- Remember infections you had in the past, so if you get the same infection again, your body’s immune system can fight it more effectively and quickly.
- Are made in your bone marrow (the spongy part in the middle of your bones), but usually live in your spleen and your lymph nodes. Some live in your thymus and blood too.
- Can travel through your lymphatic system, to any part of your body – including your skin, to fight infection or disease.
What happens when B-cells become cancerous?
CBCL develops when some of your B-cells fail to develop properly. Usually, when this happens, our immune system is able to identify that the cell has not developed properly, and it can repair or destroy those cells. Unfortunately, sometimes our immune system does not pick up on these changes, and so the B-cells continue to change until they become cancerous.
Because B-cell lymphocytes can travel to any part of your body including your skin, sometimes these cancerous changes start in your skin and develop into rashes or tumours. Although CBCL starts in your skin, some can spread to other parts of your body too.
When you have CBCL your cancerous B-cell lymphocytes:
- Will not work as effectively to fight infections and disease.
- Can become larger than they should and can look different to your healthy B-cells.
- Can cause lymphoma to develop and grow in the layers of your skin.
- Result in a rash or tumour to develop.
Overview of cutaneous B-cell lymphoma (CBCL)?
Cutaneous B-cell lymphomas (CBCL) are non-Hodgkin lymphomas (NHL) that develop in B-cells lymphocytes within the layers of your skin. Some are indolent (slow growing) and some are aggressive (fast-growing). Because CBCL starts in the layers of your skin, rather than your lymphatic system, it is called an extra-nodal lymphoma.
Symptoms of Cutaneous B-cell Lymphoma (CBCL)
The main symptom of cutaneous B-Cell lymphoma (CBCL) is a lump or lumps on your skin. The lumps may appear as small, raised, solid areas of skin that look like small pimples. These are called papules and may develop into thickened, flat areas.
Larger lumps can also develop and are often a deep red or purplish colour. These are called nodules or tumours.
Sometimes these lumps can break down and ulcerate, meaning the skin breaks down so they can become infected.




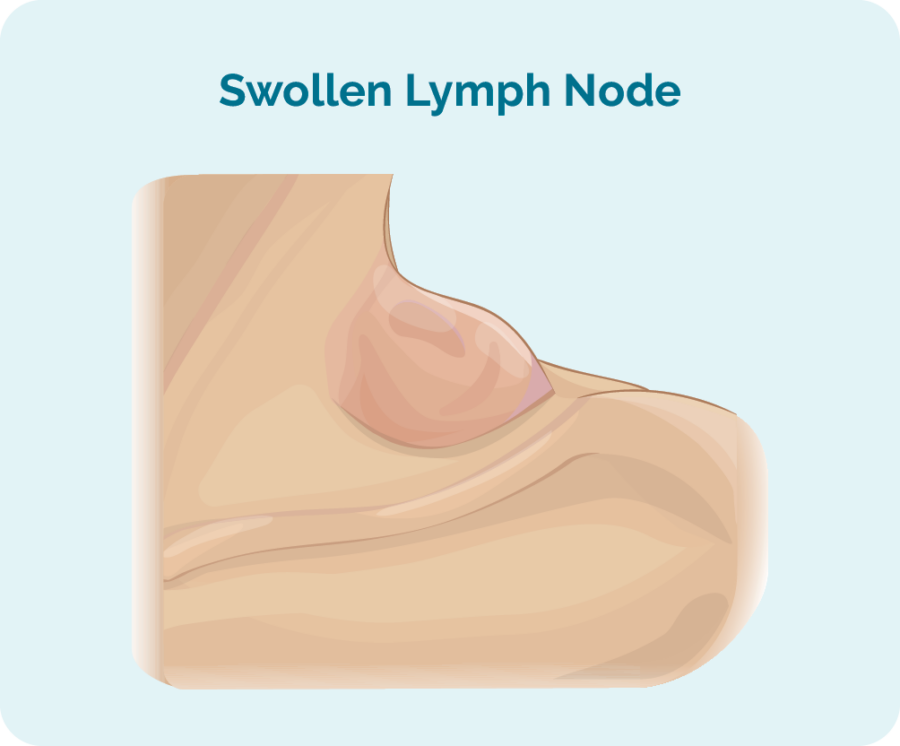
Swollen lymph nodes
You may also have swollen lymph nodes in your neck, armpits, and/or groin, which is a common symptom in many lymphomas as the cancerous B-cells can also gather in your lymph nodes.
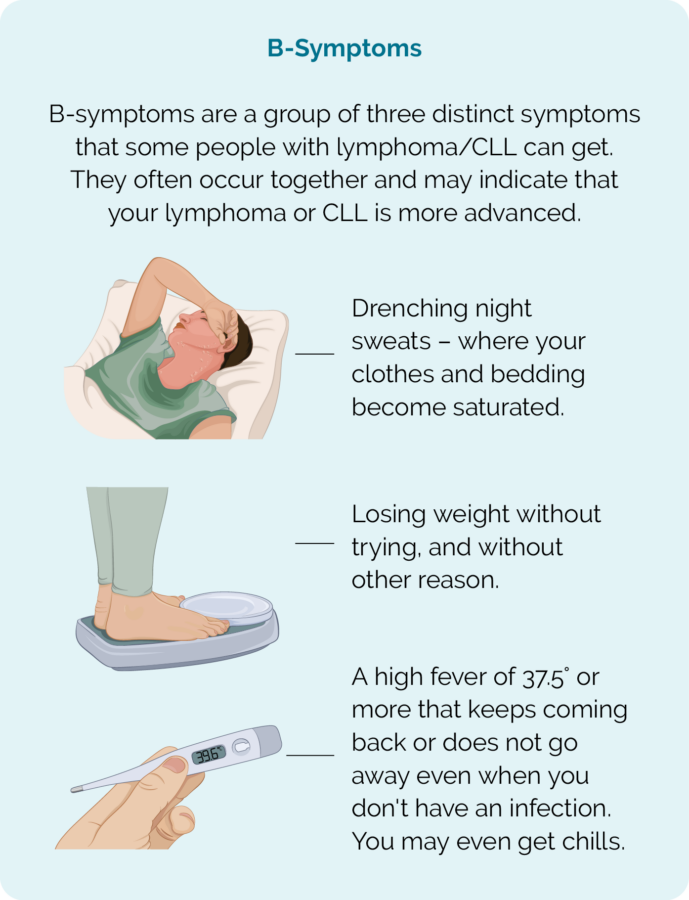
B-symptoms
Some people with lymphoma can get B-symptoms. These are a group of three symptoms that often occur together in more advanced stages of lymphoma, as the lymphoma begins to use up more of your energy to grow.
It can indicate that your lymphoma is aggressive, and you may need to start treatment soon if you get these.
B-symptoms are more common in people who have the Primary Cutaneous Diffuse Large B-cell Lymphoma-Leg Type subtype of CBCL.
Contact your doctor or healthcare team as soon as possible if you are getting this group of B-symptoms. Do not wait for your next appointment.
Diagnosis of Cutaneous B-cell lymphoma (CBCL)
You will need a skin biopsy of your rash, lump or lesions to diagnose CBCL. A biopsy is a procedure to remove the abnormal tissue so it can be looked at under the microscope by a pathologist (a specialist doctor). You will usually have a local anaesthetic to numb the area before the biopsy.
Small children may have biopsies done with a general anaesthetic so they sleep, and remain still during the procedure.
B-cell lymphoma can be difficult to diagnose and several skin biopsies may be needed before the doctor is able to confirm the diagnosis. A specialist lymphoma centre may need to assist with diagnosis of these rare lymphoma subtypes.
Subtypes of Cutaneous B-Cell Lymphoma (CBCL)
There are different subtypes of CBCL. Most are considered indolent (slow-growing) and may or may not need treatment. More aggressive – or fast-growing CBCLs will need treatment soon after you are diagnosed.
Click on the headings below to learn more about the different subtypes.
Primary Cutaneous Follicle Centre Lymphoma (PCFCL) is an indolent (slow growing) subtype of CBCL that usually affects people around the age of 60 years.
It usually develops on the back, abdomen, chest head or neck and rarely spreads anywhere else.
You may not need treatment for PCFCL because the lesions often remain stable for a long time, and some can even get better without treatment – though this rare.
If you need treatment for your PCFCL it may include radiotherapy or having the lesion surgically removed. You may also be given a corticosteroid cream to used. This usually results in a cure from the disease.
If your PCFCL is more widespread you may be offered a treatment with a monoclonal antibody called rituximab. These medications are given into your vein, and bind to the lymphoma cells. When they bind to the lymphoma cells they help your own immune system to find and destroy the lymphoma.
In some rare cases, PCFCL can transform into a faster growing subtype of lymphoma called Diffuse Large B-cell Lymphoma.
PC-MZL is an indolent subtype of CBCL and it is very rare for it spread past the skin. It is more common in people around 55 years of age.
There has been suggestion that some people of European descent that have had an infection with Borrelia Burgdorferi may have increased risk of developing this subtype of lymphoma. However, several studies have not been able to confirm this. Borrelia Burgdorferi is a bacteria related to the one that causes Lyme disease. If you do have this infection, you may be given antibiotics.
Primary Cutaneous Diffuse Large B-cell Lymphoma, Leg type is a rare and aggressive subtype of CBCL. It is more common in women than men, and in people around 75 years of age.
PC-DLBCL-LT often presents as fast-growing nodules, tumours or rash on one or both of your legs, but can spread to other parts of your body. Some people with PC-DLBCL-LT can get B-symptoms. If you get B-symptoms, make sure to let your treating team know. B-symptoms are described further down this page but can include fever, weight loss and night sweats.
Although it is a cutaneous (skin) type of lymphoma, it is often treated with the same medications as other subtypes of Diffuse Large B-Cell Lymphoma, which includes chemotherapy and a monoclonal antibody. If you have only one lesion however, you may be treated with radiotherapy. You may go into remission after your treatment, but often this type of lymphoma comes back and needs more treatment at a later time. This is called a relapse.
Epstein-Barr virus (EBV) is the virus that causes glandular fever – also known as mononucleosis (mono), or the kissing disease, because it’s transmitted through saliva.
EBV+ Mucocutaneous Ulcers are rare, but found in some people with compromised immune systems and a history of EBV infection. It is an indolent, and often self-limiting subtype of CBCL. Your risk of this rare subtype of CBCL is increased if you have had the Epstein-Barr virus and:
- have had a bone marrow, or organ transplant
- are on immune suppressive medications
- are older, and have a compromised immune system.
Most people with EBV+MCU will have one clearly defined ulcer. The ulcer may be found on the skin, gastrointestinal tract or in the mucosa of your mouth.
Treatment is often not needed, however, if you are on immune suppressing medications, your doctor may want to decrease your doses of these medications to allow your immune system to recover.
If this does not work, you may have treatment to to fight the Epstein-Barr virus, or an anti-cancer treatment called rituximab (a Monoclonal Antibody).
Staging of cutaneous B-cell lymphoma (CBCL)
When your doctor is sure you have CBCL, they will want to do more tests to see if the lymphoma is only on your skin, or if it has spread to other parts of your body.
These tests are called staging. Staging of cutaneous lymphomas is different to other subtypes of lymphoma. The staging system for cutaneous B-Cell Lymphomas is called TNM and refers to:
T = size of the Tumour – or skin lesion/s.
N = lymph Nodes involved – checks if the lymphoma has gone to your lymph nodes, and how many lymph nodes have lymphoma in them.
M = Metastasis – checks if, and how far the lymphoma has spread throughout your body.
Staging of CBCL | |
TTumour or skin affected | T1 – you only have one lesion or tumour. T2 – you have more than one skin lesion, but the lesions are either in one area, or two areas close together on your body. T3 – you have lesions or tumours across many areas of your body. |
NLymph Nodes | N0 – your lymph nodes appear normal. N1 – one group of lymph nodes are involved. N2 – two or more groups of lymph nodes are affected in your in your neck, above your clavicle, underarms, groin or knees. N3 – lymph nodes in, or near your chest, lungs and airways, major blood vessels (aortic) or hips are involved. |
MMetastasis (spread) | M0 – none of your lymph nodes are affected. M1 – lymphoma has spread to your lymph nodes outside of your skin. |
Staging scans and tests
The scans and tests needed for staging and before treatment can start may include:
- Positron emission tomography (PET) scan
- Computed tomography (CT) scan
- Bone marrow biopsy (many people with CBCL will not need this but some may, particularly if you have an aggressive subtype)
Other tests you may need
As well as your biopsy and staging tests you will also need other tests if you are going to have treatment. These tests are called “baseline tests” and are used to check your overall health. Depending on the subtype of your CBCL and the planned treatment you may have one or more of these tests.
You will have these same tests throughout your treatment, and they will be checked against your baseline tests before treatment. This helps your doctor make sure your body is coping with the treatment you are getting.
Baseline tests may include:
- Physical examination
- Vital observations (blood pressure, temperature, & pulse rate & oxygen levels).
- Heart scan.
- Kidney scan.
- Breathing tests.
- Blood tests.
Waiting for Results
Expect to wait several weeks to have all your tests and get the results back. This waiting time can be difficult for some people. It can help to have someone to talk to during this time. If you have a family member or friend you can reach out to, let them know what’s going on and what you need from them.
People often want to help, but don’t quite know what to do, or don’t want to impose. Letting them know what you need helps them and you.
If your symptoms get worse while waiting for results, or you start getting new symptoms including B-symptoms as listed above, let your doctor know.
Your treating team will be able to offer you advice on how best to manage your symptoms while waiting for results.
Contact us
You can also contact our Nurse Hotline to talk to one of our Lymphoma Care Nurses. Just click on the Contact us button at the bottom of this page. We can help by sending you information or letting you know what support is available. You may also like to join one of our social media pages to chat with other people living with lymphoma (see the social media links at the top of this page).
Treatment of cutaneous B-cell lymphoma (CBCL)
If you need treatment for your CBCL, your doctor will consider several things when deciding the best treatment options for you. These will include:
- The stage and size of your lymphoma
- Any symptoms you are getting
- How the lymphoma is affecting your body
- Your age and general health and well-being (including any other illnesses you may have and treatments you are having)
- Your preferences for treatment once you have been given all the information.
Standard first-line treatment for indolent (slow-growing) cutaneous B-cell lymphomas
There are many different types of treatment for CBCL. Depending on your individual situation, subtype and stage you may be offered any of the below.
- Antibiotics – If you have Cutaneous Marginal Zone Lymphoma and also have an infection with Borrelia burgdorferi, you may only need antibiotics. By killing the bacteria the lymphoma feeds off, it is thought the lymphoma will starve and die. However the evidence for this is limited.
- Surgery – You may be able to have a lesion completely removed with surgery. In some cases you may also be offered radiotherapy after the surgery to ensure any lymphoma cells left behind are destroyed.
- Radiotherapy on its own if there are a few lesions
- Topical corticosteroids
- Topical chemotherapy such as Nitrogen mustard and carmustine
- Immune response modifiers such as Imiquimod
- Retinoids such as Bexarotene
- Phototherapy
- PUVA phototherapy
- ‘Watch and wait’ if there are no troublesome symptoms
- Chlorambucil
- Rituximab
- Rituximab and Bendamustine
- R-CVP (Rituximab, cyclophosphamide, vincristine, and prednisolone)
Standard first-line treatment for aggressive cutaneous B-cell lymphomas
- Chemotherapy followed by Radiotherapy
- CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone)
- R-CHOP (Rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone)
- Stem cell transplantation -allogeneic
Common side effects of treatment
There are many different side effects of the treatment and these are dependent on the treatment that has been given. The treating doctor and/or cancer nurse can explain the specific side effects prior to the treatment. Some of the more common side effects of treatment may include:
- Anaemia (low red blood cells carry oxygen around the body)
- Thrombocytopenia (low platelets that help bleeding and clotting)
- Neutropenia (low white blood cells help with immunity)
- Nausea and vomiting
- Bowel problems such as constipation or diarrhoea
- Fatigue (tiredness or lack of energy
The medical team, doctor, cancer nurse or pharmacist, should provide information about:
- What treatment will be given
- What are the common and possible side effects for the treatment
- What side effects do you need to report to the medical team
- What are the contact numbers, and where to attend in case of emergency 7 days a week and 24 hours per day
Prognosis of cutaneous B-cell lymphoma (CBCL)
Cutaneous follicle centre lymphoma (slow-growing) and cutaneous marginal zone B-cell lymphoma (slow-growing) both have a good prognosis. They are often diagnosed early, grow slowly, and respond well to treatment.
Cutaneous diffuse large B-cell lymphoma, leg type behaves as an aggressive (fast-growing) lymphoma They do respond to treatment but are highly likely to relapse (come back).
Follow-up care
Once treatment has completed, post treatment staging scans are done to review how well the treatment has worked. The scans will show the doctor if there has been a:
- Complete response (CR or no signs of lymphoma remain) or a
- Partial response (PR or there is still lymphoma present, but it has reduced in size)
If all goes well regular follow-up appointments will be made for every 3-6 months to monitor the below:
- Review the effectiveness of the treatment
- Monitor any ongoing side effects from the treatment
- Monitor for any late effects from treatment over time
- Monitor signs of the lymphoma relapsing
These appointments are also important so that the patient can raise any concerns that they may need to discuss with the medical team. A physical examination and blood tests are also standard tests for these appointments. Apart from immediately after treatment to review how the treatment has worked, scans are not usually done unless there is a reason for them. For some patient’s appointments may become less frequent over time.
Relapsed or refractory management of CBCL
If Indolent cutaneous B-cell lymphoma relapses (comes back) after treatment, it can still be successfully treated with another treatment.
Cutaneous B-cell lymphoma leg type can be treated with different combination chemotherapies.
Treatments under investigation for CBCL
There are many treatments that are currently being tested in clinical trials in Australia and around the world for patients with both newly diagnosed and relapsed lymphoma. Some of the treatments for CBCL can include:
- Panobinostat (Farydak)
- Lenalidomide (Revlimid)
- Bendamustine (Treanda)
What happens after treatment?
Late Effects
Sometimes a side effect from treatment may continue or develop months or years after treatment has completed. This is called a late effect.
Finishing treatment
This can be a challenging time for many people and some of the common concerns can be related to:
- Physical
- Mental wellbeing
- Emotional health
- Relationships
- Work, study, and social activities
Survivorship - Living with and after cancer
A healthy lifestyle, or some positive lifestyle changes after treatment can be a great help to your recovery. There are many things you can do to help you live well with DLBCL.
Many people find that after a cancer diagnosis, or treatment, that their goals and priorities in life change. Getting to know what your ‘new normal’ is can take time and be frustrating. Expectations of your family and friends may be different to yours. You may feel isolated, fatigued or any number of different emotions that can change each day.
The main goals after treatment for your DLBCL is to get back to life and:
- be as active as possible in your work, family, and other life roles
- lessen the side effects and symptoms of the cancer and its treatment
- identify and manage any late side effects
- help keep you as independent as possible
- improve your quality of life and maintain good mental health
Different types of cancer rehabilitation may be recommended to you. This could mean any of a wide range of services such as:
- physical therapy, pain management
- nutritional and exercise planning
- emotional, career and financial counselling.
