Overview of Hodgkin lymphoma (HL) in children
Hodgkin lymphoma (HL) is an aggressive (fast growing) B-cell lymphoma. Lymphoma and is the 3rd most common cancer in Australian children and young people aged 0 – 14 years after leukaemia and brain or central nervous system (CNS) cancer. HL accounts for around 7% of all childhood cancers (0-14 years) and around 40% of all lymphomas for this age group. The disease affects around 30 Australian children each year.
It is twice as common in boys than it is girls at this age. Lymphoma is very rare in younger children, but it becomes more common in older children (10-14 years) and increases with age. HL is the most common cancer impacting young people aged 15-29 years. There is an increased later life incidence in older adults over 70 years, although HL can occur at any age.
HL has an excellent prognosis, where over 90% of children are cured after standard first-line treatment. Most research is currently studying how to reduce late effects, or side effects from cancer treatment that can leave lasting side effects or chronic health conditions months to years after treatment.
What is Lymphoma?
Lymphomas are a group of cancers of the lymphatic system. They develop when lymphocytes, which are a type of white blood cell that normally fight infection as part of the body’s immune system, gain DNA mutations. These affected cells then divide and grow uncontrollably or do not die when they should, resulting in lymphoma. There are two main types of lymphoma, Hodgkin lymphoma and non-Hodgkin lymphoma(NHL). Lymphomas are further divided into:
- Indolent (slow growing) lymphoma
- Aggressive (fast-growing) lymphoma
- B-cell lymphoma develop from abnormal B-cell lymphocytes & are the most common, accounting for around 85% of all lymphomas (all ages)
- T-cell lymphoma develop from abnormal T-cell lymphocytes and account for around 15% of all lymphomas (all ages)
Hodgkin lymphoma (HL) is usually an aggressive (fast growing) B-cell lymphoma. HL accounts for approximately 40% of all childhood lymphoma cases diagnosed each year.
It is called Hodgkin lymphoma because:
- It develops from abnormal B-cell lymphocytes
- Hodgkin lymphoma was named after the doctor who first described the condition named Dr Thomas Hodgkin (in 1832)
- In Hodgkin lymphoma, a particular type of abnormal cell, that is unusually large, malignant (cancerous) mature B-cell called Reed-Sternberg cells (named after the two scientists who discovered it), can be seen under the microscope in tissue samples.
- Non-Hodgkin lymphomas do not contain this type of cell
- All lymphomas that were discovered after Hodgkin lymphoma, were called non-Hodgkin lymphomas, that accounts for 90% of all lymphomas, that all have different characteristics and treatment
There are two main types of Hodgkin lymphoma that are treated and managed differently. These include:
Classical Hodgkin lymphoma, that is the more common type of disease, characterised by the presence of large abnormal Reed-Sternberg cells
Nodular lymphocyte predominant Hodgkin lymphoma, is a rare subtype involving variants of Reed-Sternberg cells called “popcorn” cells because of their appearance.
Who is affected by Hodgkin lymphoma (HL)?
Hodgkin lymphoma (HL) can occur at any age, but it is the most common cancer in adolescents and young adults, with around a third of cases occurring in the 15-29 years age group. There is another peak in incidence in those over 70 years of age.
Lymphoma accounts for 7% of childhood cancers, it is the third most common cancer in children aged 0-14 years, behind leukaemia and brain or central nervous system (CNS) cancers. HL accounts for 40% of lymphoma cases in children, accounting for around 30 Australian children a year diagnosed. It becomes more common in older children (10-14 years).
Having a child diagnosed with lymphoma can be an incredibly stressful and emotional experience, there is no right or wrong reaction.
Types of Hodgkin lymphoma (HL) in children
There are two main types of Hodgkin lymphoma (HL) that include:
Classical Hodgkin lymphoma (Chl):
cHL isthe most common subtype of Hodgkin lymphoma and is characterised by the presence of large, abnormal Reed-Sternberg cells.
Classical Hodgkin lymphoma (cHL) is further divided into 4 histologic subtypes according to:
- Number and morphology of Reed-Sternberg cells seen under the microscope
- The cellular background in the biopsied sample that can be seen under the microscope
Mixed cellularity classical Hodgkin lymphoma (cHL) accounts for approximately 30-35% of all cHL cases. This subtype is more common in men than women and typically affects older adults. Common sites at presentation include abdominal lymph nodes and spleen. Can be confused with peripheral T-cell lymphoma.
Lymphocyte depleted classical Hodgkin lymphoma (cHL) is the rarest subtype accounting for less than less than 5% of cHL cases. It occurs more commonly in HIV-infected or EBV-infected patients. This subtype frequently occurs in the bone marrow (up to 75% of cases). It is rarely diagnosed. Frequently misdiagnosed with non-Hodgkin anaplastic large cell lymphoma.
Lymphocyte rich classical Hodgkin lymphoma (cHL) accounts for less than 1 percent of all cHL cases. This subtype of cHL is typically diagnosed at an earlier stage than other subtypes of cHL and has a very low relapse (comes back) rate. It is difficult to differentiate this subtype from nodular lymphocyte predominant Hodgkin lymphoma as they have similar presentation and prognosis.
Nodular lymphocyte predominant Hodgkin lymphoma:
Nodular lymphocyte predominant Hodgkin lymphoma involves variants of Reed-Sternberg cells called ‘popcorn’ cells.
Nodular sclerosis classical Hodgkin lymphoma (cHL)
Is the most common subtype in children accounting for about 40-50 percent of all cHL cases. it affects females more than males. This subtype receives its name from its appearance under the microscope with nodular referring to a ‘node-like’ pattern in the tissue and sclerosis referring to ‘scar tissue’ as there is typically a mixture of Reed-Sternberg cells, normal white blood cells and scar tissue. This subtype often presents in the mediastinum (chest area).
Nodular Lymphocyte Predominant Hodgkin lymphoma is typically slower growing than the classical types of Hodgkin lymphoma, it resembles other types of non-Hodgkin lymphoma which are also slow-growing, and it is therefore treated differently to the classical types of Hodgkin lymphoma.
Symptoms of Hodgkin lymphoma (HL)
The first symptoms of HL is a lump or several lumps that don’t go away after several weeks. You might feel one or more lumps on your child’s neck, armpit or groin. These lumps are swollen lymph nodes, where abnormal lymphocytes are growing. These lumps often start in one part of a child’s body, usually the head, neck or chest and then tend to spread in a predictable manner from one part of the lymphatic system to the next. In advanced stages, the disease can spread to the lungs, liver, bones, bone marrow or other organs.
The common symptoms of Hodgkin lymphoma include:
- Painless swelling of lymph nodes in the neck, underarm, groin or chest
- Shortness of breath – due to enlarged lymph nodes in the chest
- Cough (usually dry cough)
- Fatigue
- Difficulty recovering from an infection
- Itchy skin (pruritus)
B symptoms are what doctors call the following symptoms and some children may have these and they can include:
- Night sweats (especially at night, where you might need to change their sleepwear and bedding)
- Persistent fevers
- Unexplained weight loss
It is important to note that many of these symptoms are related to causes other than cancer and are sometimes difficult for doctors to diagnose.
Diagnosis of Hodgkin lymphoma (HL)
A biopsy is always required for diagnosis of lymphoma. A biopsy is a surgical procedure to remove part of or all of an affected lymph node or other tissue to look under the microscope by a pathologist to see what the cells look like. The biopsy is usually done under general anaesthetic for children to help reduce distress.
An excisional node biopsy is the best investigative option, as it collects the most adequate amount of tissue to be able to do the necessary testing for a diagnosis.
Waiting for results can be a difficult time. It may help to talk to family, friends or a specialist nurse.
Staging of Hodgkin lymphoma (HL)
Once a diagnosis of Hodgkin lymphoma (HL) is made, further tests are required to see where else in the body the lymphoma is located or has affected. This is called staging. The staging of lymphoma helps the doctor to know what the best treatment will be for your child.
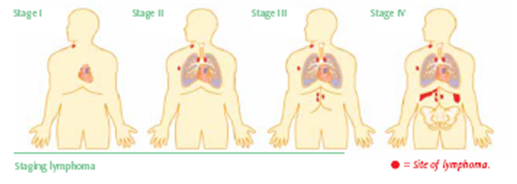
There are four stages from stage 1 (lymphoma in one area) through to stage 4 (lymphoma that is widespread).
- Early stage means stage 1 and some stage 2 lymphoma. This may also be referred to as ‘localised’. Stage 1 or 2 means that the lymphoma is found in one area or a few areas close together.
- Advanced stage means the lymphoma is stage 3 and stage 4, and it is widespread lymphoma. In most cases, the lymphoma has spread to parts of the body that are far from each other.
‘Advanced’ stage lymphoma does sound concerning, but lymphoma is what is known as a systemic cancer. It can spread throughout the lymphatic system and nearby tissue. This is why systemic treatment (chemotherapy) is needed to treat Hodgkin lymphoma.
Staging scans and tests
Some of the tests needed can include:
- Blood tests (such as: full blood count, blood chemistry and erythrocyte sedimentation rate (ESR) to look for evidence of inflammation)
- Chest x-ray – these images will help identify presence of disease in the chest
- Positron emission tomography (PET) scan – done to understand all active sites of disease in the body before treatment starts
- Computed tomography (CT) scan
- Bone marrow biopsy (only usually done in some patients if there is evidence of advanced disease)
A number of baseline tests prior to any treatment may also be used to check organ function. These are often repeated during and after treatment has completed to assess whether the treatment has affected the function of any organs. Sometimes the treatment and follow-up care may need to be adjusted to help manage any adverse side effects. These may include.
- Physical examination
- Vital observations (Blood pressure, temperature & pulse rate)
- Heart scan
- Kidney scan
- Breathing tests
Many of these staging and organ function tests are done again after treatment to check whether the lymphoma treatment has worked and to monitor the effect treatment has had on the body.
Prognosis of Hodgkin lymphoma (HL)
Both classical and nodular lymphocyte predominant Hodgkin lymphoma are highly curable, with survival rates over 90%. Those who do not respond completely to standard first-line treatment or relapse, can still have treatments available to potentially cure the disease. Many of the current studies are looking at ways to maintain a high cure rate but reducing the long-term side effects that the treatment may cause.
Treatment of Hodgkin Lymphoma (HL)
Once all of the results from the biopsy and the staging scans have been completed, the doctor will review these to decide the best possible treatment for your child. At some cancer centres, the doctor will also meet with a team of specialists to discuss the best treatment option. This is called a multidisciplinary team meeting (MDT) meeting.
Your doctors will take into consideration many factors about their lymphoma and general health to decide when and what treatment is required. This is based on:
- The stage of the lymphoma
- Symptoms at diagnosis
- Past medical history
- General health
- Current physical and mental wellbeing
- Your preferences
The chemotherapy protocols used to treat adult patients with Hodgkin lymphoma are different to the protocols used to treat children, although many of the chemotherapy and other cancer medicines are similar. The treatment of Hodgkin lymphoma in young people aged from around 15-18 years may also differ depending on whether they are referred for treatment by their GP to a children’s hospital or to an adult hospital. This will be explained further in the young people and Hodgkin lymphoma.
The treatment and management for nodular lymphocyte predominant Hodgkin lymphoma (NLPHL)is different to that of classical Hodgkin lymphoma and therefore will be discussed separately.
Treatment of classical Hodgkin lymphoma (cHL)
Since classical Hodgkin lymphoma (cHL) is a rapidly growing lymphoma, treatment may need to start soon after a diagnosis is made. The standard treatment for patients with cHL is a combination of chemotherapy, with some patients also receiving radiotherapy after chemotherapy.
The doctor may recommend one of the following standard first-line treatments for paediatric classical Hodgkin lymphoma:
- COG-ABVE-PC (doxorubicin, bleomycin, vincristine, etoposide, cyclophosphamide and prednisolone) are administered every 21 days for 4-6 cycles.
- Bv-AVECP (brentuximab vedotin, doxorubicin, vincristine, etoposide, cyclophosphamide and prednisolone)
- Radiotherapy may be given in some children as required after chemotherapy
Treatment of nodular lymphocyte predominant Hodgkin lymphoma (NLPHL)
The treatment for nodular lymphocyte predominant Hodgkin lymphoma (NLPHL) is treated very differently than classical Hodgkin lymphoma (cHL). Depending on the stage of the disease different treatments are indicated.
Early Stage NLPHL:
- Watch and wait active monitoring until symptoms need to be treated
- Radiotherapy only
- Rituximab – this drug is administered intravenously, and it is a monoclonal antibody which targets B-cells and has worked very well to treat other types of B-cell lymphoma.
- AVPC (doxorubicin, vincristine, prednisone, & cyclophosphamide)
- CVP (cyclophosphamide, prednisone, & vincristine)
- Clinical trial participation
Advanced NLPHL:
- Rituximab
- ABVD (doxorubicin, bleomycin, vinblastine & dacarbazine) – given over one day 1 & 15 of each 28-day cycle (4-6 cycles) plus rituximab, with or without radiotherapy
- R-CHOP (cyclophosphamide, doxorubicin, vincristine, rituximab & prednisolone)
- Radiotherapy +/- after chemotherapy
- ABVE-PC (doxorubicin, bleomycin, vincristine, etoposide, prednisone, procarbazine) with or without radiotherapy for paediatric patients
Common side effects of treatment
There are many different side effects of the treatment, that is individual for each treatment regimen. The treating doctor and/or cancer nurse will explain these to you prior to your child starting treatment.
Some of the more common side effects of treatment can include:
- Neutropenia (low type of white blood cell that helps to fight infection)
- Thrombocytopenia (low platelets that help with clotting or bleeding)
- Anaemia (low red cells that help provide oxygen to your body)
- Nausea and vomiting
- Bowel problems (constipation or diarrhea)
- Fatigue (tiredness or lack of energy)
The medical team, doctor, cancer nurse or pharmacist, should provide you with information about the treatment, the common side effects, what symptoms to report and who to contact. If not, please ask these questions when you are about to leave the cancer centre.
Fertility preservation
The treatment for Hodgkin lymphoma can affect your child’s fertility. Although many males and females go on to have children later in life after treatment, it is important that you discuss the risks on their fertility and what is available to help preserve their fertility before treatment starts.
Follow-up care
Once treatment has completed, your child will have post treatment staging scans to review how well the treatment has worked and if there is a complete response (CR or no signs of lymphoma remain) or partial response (PR or there is still lymphoma present, but it has reduced in size).
If a complete remission has been achieved there will be follows ups with the doctor usually every 3-6 months. These appointments are important so that the medical team can check how well the recovery is from treatment. They are also a good opportunity for you to talk to the doctor or nurse about any concerns you may have. The medical team will want to know how your child is feeling both physically and mentally, and to:
- Review the effectiveness of the treatment
- Monitor any ongoing side effects from the treatment
- Monitor for any late effects from treatment over time
- Monitor signs of the lymphoma relapsing
Physical examination and blood tests for these appointments and apart from immediately after treatment to review how the treatment has worked, scans are not usually done unless there is a particular reason for them. If your child stays well, their appointments may become less frequent over time.
Relapsed or refractory classical HL
Relapsed lymphoma is when the cancer has come back, refractory lymphoma is when the cancer is not responding to standard treatment. For some children and young people, classical Hodgkin lymphoma returns and in some rare cases it does not respond to initial treatment (refractory). For these patients there are other treatments that can be successful, and may include:
- High dose combination chemotherapy followed by autologous stem cell transplant (small groups of patients may receive an allogeneic stem cell transplant)
- Combination chemotherapy
- Immunotherapy
- Radiotherapy
- Clinical trial participation
When a patient is suspected to have relapsed disease, often the same staging exams are done, which include the tests that were stated above in the diagnosis and staging section.
Relapsed or refractory treatment for NLPHL
- Clinical trial participation
- Watch & wait: active surveillance if recurrence is limited and there are no symptoms
- ABVD-R (doxorubicin, bleomycin, vinblastine, dacarbazine & rituximab)
- +/- radiotherapy after chemotherapy
- Combination chemotherapy
- Radioimmunotherapy (RIT)
Treatment under Investigation
There are many new treatments that are currently being tested in clinical trials around the world for patients with both newly diagnosed and relapsed lymphoma. Some of the treatments being investigated in clinical trials include:
- Bendamustine (RibomustinTM)
Given the high survival rate for patients with Hodgkin lymphoma, many research studies now focus on learning how to eliminate potential late effects e.g. Secondary cancers or chronic medical conditions) while maintaining excellent outcomes. This involves trying to determine when some treatments designed to direct the immune system against specific cancer cells, called immunotherapy, are currently being studied.
What happens after treatment?
Late effects
Sometimes a side effect from treatment may continue or can develop months or years after treatment has completed. This is called a late effect.
Children and adolescents may have treatment-related side effects that can appear months or years after treatment, including problems with bone growth and development of sex organs in males, infertility, and thyroid, heart and lung diseases.
Some patients who survive childhood Hodgkin lymphoma may develop a secondary cancer after diagnosis, primarily breast cancer, non-Hodgkin lymphoma, thyroid cancer or acute leukaemia, sometimes many years later. Many current treatment regimens and research studies now focus on trying to decrease the risk for these late effects.
For these reasons it is important the survivors of Hodgkin lymphoma receive regular follow-up and monitoring. It is also important that young people find a good GP that they can see regularly.
