What is Hepatosplenic Gamma Delta T-cell Lymphoma?
HepatoSplenic Gamma Delta T-cell Lymphoma (HSGDTL) is a very aggressive subtype of Non-Hodgkin Lymphoma. Aggressive is a term used to describe a lymphoma that grows and spreads very quickly. It is very rare, with only about 200 cases being reported on throughout the world, in the past 30 years.
SHGDTL is named to describe where the lymphoma is mostly found and the features of the lymphoma cells:
- Hepato refers to the liver.
- Splenic refers to the spleen.
- Gamma refers to a type of receptor (or marker) found on the cell.
- Delta refers to a type of receptor (or marker) found on the cell.
- T-cell refers to the type of cell that becomes cancerous – T-cell lymphocytes.
So, this is a cancer of T-cell lymphocytes that have specific receptors called gamma and delta on them, and affects primarily your liver and spleen.
What are T-cell Lymphocytes?
T-cell lymphocytes are an important part of our immune system that protect us against infection and disease, and regulate our immune system to prevent autoimmune attacks. Auto immune attacks happen when our immune system is overactive or faulty and begins to fight our own body instead of infection and disease.
About T-cell Lymphocytes
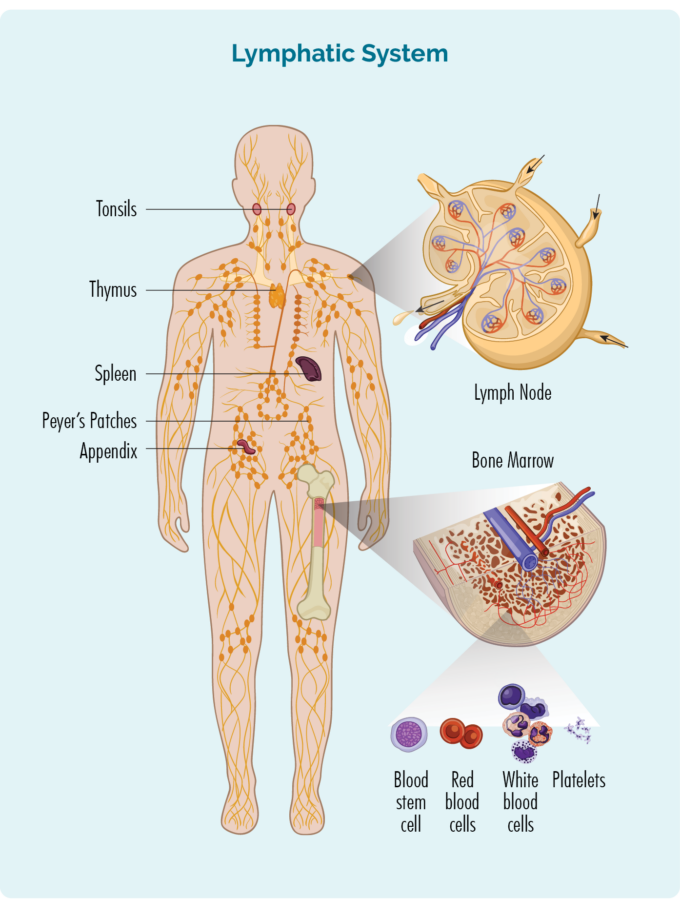
- T-cells are made in our bone marrow, mature in our thymus, but can live in any part of our lymphatic system – including our spleen and lymph nodes (see picture).
- Most T-cells need to be activated to work effectively. They are usually resting in our thymus or other parts of our lymphatic system, and only wake up and fight infection when other immune cells let them know there is an infection or disease to fight. When they wake up, T-cells can travel to any part of our body to fight the infection or disease.
- Some T-cells are responsible for “regulating” the immune response. This means that once an infection has been destroyed, the “Regulatory T-cells” tell other immune cells to “stand down” so they don’t keep fighting and cause harm to our good cells.
- Natural Killer (NK) cells are often called “NK T-cells”. They are specialised immune cells that recognise and destroy cancer cells. Unlike other T-cells, NK cells do not need to be activated to fight cancer. They are ready to fight at all times, and actively move around your body on the look-out for cells that have cancerous changes.
- After fighting an infection or disease, some T-cells become “Memory T-cells”. They remember everything there is to know about the infection and how to fight it. That way, if we ever get the same infection or disease again, our immune system can fight it a lot more quickly and effectively.
- Some T-cells help other immune cells, such as B-cell lymphocytes to work effectively. These T-cells are called “Helper T-cells”.
- When we have an infection, Helper T-cells activate another type of T-cell called “Cytotoxic T-cells” and once activated Cytotoxic T-cells fight infection and disease. When not activated, Cytotoxic T-cells rest in our thymus, spleen and other parts of our lymphatic system.
Hepatosplenic Gamma Delta T-cell Lymphoma is a cancer of "Cytotoxic T-cells" - most commonly, resting Cytotoxic T-cells.
Causes of Hepatosplenic Gamma Delta T-cell Lymphoma
As with most lymphomas we don’t know what causes HSGDTL. It seems to be more common in teenagers and young adults but can also affect children and older adults.
Unlike many other lymphoma, Epstein Barr Virus (EBV), the virus that causes glandular fever does not seem to have any link to this subtype. However, there are some risk factors that may increase your chance of developing HSGDTL. These include:
- Long term inflammation, such as what happens with inflammatory bowel disease or other inflammatory disorders.
- Having a disorder of your immune system that makes you more prone to infection and disease (immunocompromised).
- Medication that weakens your immune system (immunosuppression), such as those taken for autoimmune diseases or after an organ transplant.
Symptoms of Hepatosplenic Gamma Delta T-cell Lymphoma (HSGDTL)
HSGDTL is difficult to diagnose because many symptoms are similar to symptoms of different conditions, and only a few are typical of lymphoma.
Unlike most lymphomas, you may not have any swollen lymph nodes. The most common symptoms of HSGDTL include:
- Very swollen (enlarged) spleen. This is called splenomegaly and can cause pain or discomfort in the middle or toward the left side of your chest or abdomen and feeling of fullness even if you haven’t eaten much.
- Enlarged liver. This is called hepatomegaly, and can cause pain or discomfort in the middle or toward the right side of your chest or abdomen and feeling of fullness even if you haven’t eaten much. You may even get pain in your right shoulder and yellowing of your skin and eyes.
(when your liver and spleen are both enlarged it is called hepatosplenomegaly).
- Infiltrates of cancerous T-cells in your bone marrow, causing low red blood cells (anemia), low platelets (thrombocytopenia). In some cases you may have low neutrophils (neutropenia). These changes can cause dizziness, shortness of breath, severe fatigue, bleeding or bruising more than usual and infections.
- Skin rash or itchy skin.
- In more advanced stages of HSGDTL you may have high lymphocytes in your blood tests.
- Severe fatigue (tiredness) and general weakness.
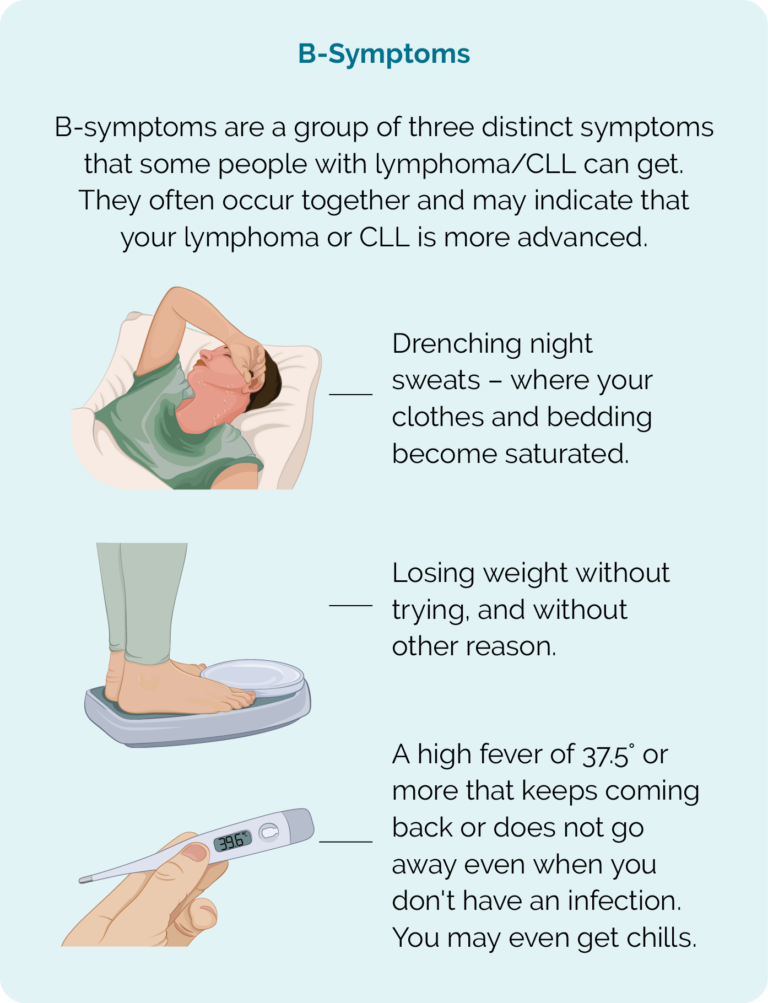
- B-symptoms.
How is HSGDTL diagnosed?
HSGDTL is very aggressive, so symptoms usually start and get worse over a period of weeks. Most people go to the doctor unwell and may at first be given antibiotics to treat a suspected infection.
When antibiotics don’t work, and symptoms get worse more tests may be done. You may be sent for blood tests, an ultrasound scan or CT scan to check your blood, liver, spleen and other organs. Your doctor may suspect you have a cancer if these scans and tests come back abnormal.
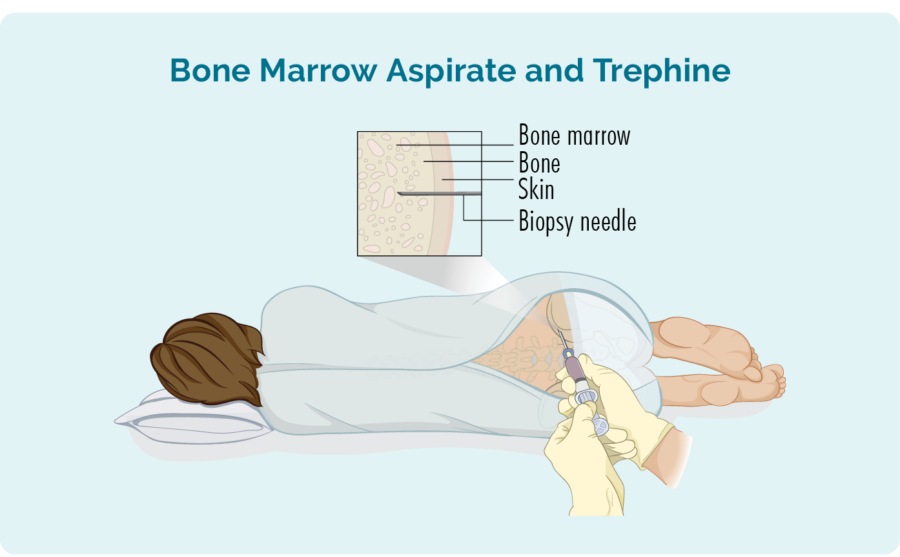
To diagnose HSGDTL you will likely need several biopsies including a bone marrow biopsy, liver biopsy and possibly a spleen biopsy. A biopsy is when a part of the affected tissue (suspected of having cancer in it) is removed and sent to pathology for testing. The pathologist will look at:
- what part of the organ the cancerous cells are growing
- the type of cell that has become cancerous (such as a cytotoxic T-cell)
- what proteins or receptors are on the cancerous cells.
Treatment
Due to this type of lymphoma being so rare, there are no standardised treatment options. It does not usually respond as well to chemotherapy treatments as other subtypes of aggressive lymphoma.
If your lymphoma does respond well to the chemotherapy, and you go into remission, it is very likely that you relapse. A relapse is when the lymphoma comes back. After a relapse, you may need more treatment, which is called second-line treatment.
In some cases, you may have chemotherapy to control the disease followed by higher dose chemotherapy to eliminate the lymphoma followed by stem cell transplant. The stem-cell transplant is needed after higher dose chemotherapy to replace your good healthy cells, and may offer a greater chance of remission, and possibly, though rarely, a cure.
Chemotherapy
Chemotherapy is given as part of a protocol, often with a combination of different types of chemotherapy medicines. It is given in cycles, meaning you will have chemotherapy, then a rest period of a 2 or 3 weeks then more chemotherapy. You may have 6 or more cycles of the same protocol, or you may have 1 or 2 cycles of one protocol and then swap to a different protocol.
Australasian Lymphoma Alliance
With such a rare subtype of lymphoma you may wonder how your haematologist or oncologist will know how to pick the best treatment option for you. The Australasian Lymphoma Alliance (ALA) is a network of highly experienced haematologists and researchers from Australia and Asia Pacific who have a special interest in lymphoma.
Within ALA there is a specialised group who focus on rare T-cell lymphomas. Your doctor is able to present your case to these specialists to learn about new clinical trials and treatment options, and get advice if needed on the best options for you.
Multidisciplinary meetings
Your treating haematologist or oncologist may also meet with other haematologists, nurses and allied health professionals within your hospital or district. Together they look at your individual situation, and put a plan together to make sure all your needs are met.
Common chemotherapy protocols
The below are some of the protocols you may be offered. Once you know which protocol you will be having, click on the below names to find more information on that protocol.
- CHOP
- CHOEP
- Hyper CVAD Part A and Part B
- DHAP
- DHAC
- GDP
- Pralatrexate
- Romidepsin (not funded)
For more information on stem-cell transplants, click on the download button below.
You may be offered a treatment option not listed above. As new medications are approved, or clinical trials reveal other treatment options you may have access to different medicine and treatments. You may also be offered the opportunity to join a clinical trial.
Clinical trials
Clinical trials are an important way to find new treatments, or combinations of treatments to improve outcomes for patients with lymphoma. They can also offer you the opportunity to try new types of treatment that have not previously been approved for your type of lymphoma.
HepatoSplenic Gamma Delta T-cell Lymphoma is a subtype of Peripheral T-cell Lymphoma which are a group of Non-Hodgkin Lymphoma. This means you may be eligible for clinical trials for people with:
- T-cell lymphoma
- Peripheral T-cell Lymphoma
- Hepatosplenic Gamma Delta T-cell Lymphoma
- Hepatosplenic T-cell lymphoma
- Aggressive Non-Hodgkin Lymphoma
- Relapsed or refractory lymphomas (if you have relapsed or refractory lymphoma).
If you are interested in joining a clinical trial, ask your haematologist or oncologist if there are any you are eligible for. Not all trials are run at every hospital, or even in every state, so if you are willing to travel, let your doctor know how far you are willing to travel (including if you willing to travel to another country) for a trial.
New trials are starting all the time, so even if you asked before, you can always ask again. It is recommended that you ask about clinical trials anytime you need to start a new treatment.
Other treatment options
When you have a rare lymphoma with no standard treatment protocol, it is always worth asking your doctor if there are any “off label treatments”, “compassionate access schemes” or “copay options” that may provide an opportunity to have a treatment that would not otherwise be available to you.
Watch the video with Professor Michael Dickinson about alternative access to medicines.
What happens when lymphoma is refractory or relapses?
Unfortunately, it is not uncommon for this subtype of lymphoma to be refractory to treatment or to relapse. Refractory means it does now work as effectively as hoped, and does not control your lymphoma.
A relapse happens when treatment worked well and put you into remission, meaning there were no, or very little signs of lymphoma left in your body. However, after a time of remission, the lymphoma comes back.
When this happens, you may be offered some of the above treatments again. But you should ask if there are any clinical trials that you would be eligible for, or if there are any off label or compassionate access schemes to help you access other medicines or treatments.
For more information on relapsed and refractory lymphoma, as well as extra supports you can get, click on the link below.
What happens after treatment?
Your doctor will want to still see you regularly after your treatment ends to monitor your progress and make sure you have no signs of relapse, or late effects.
Late Effects
Sometimes a side effect from treatment may continue or develop months or years after treatment has completed. This is called a late effect. Your doctor will continue to monitor you after you finish treatment to pick up any late effects early so they can be managed appropriately. The type of late effects you get will depend on the type of treatment you had.
Make sure you ask your doctor what late-effects to expect and when and how you should report to them.
Summary
- Hepatosplenic Gamma Delta T-cell Lymphoma is a very rare, aggressive and difficult to diagnose subtype of Non-Hodgkin Lymphoma.
- It is more common in young people up to the age of around 35 years of age but can affect children and older adults too.
- Due to the rareness of this subtype, there are no standardised treatment protocols, and it typically does not respond as well to standard chemotherapy as other types of lymphoma.
- High-dose chemotherapy followed by a stem-cell transplant offers a better chance at remission.
- You may be able to access other types of treatment through clinical trials or compassionate access schemes.
- It is common for this subtype of lymphoma to relapse and need treatment more than once.
- For more information on your lymphoma, treatment or support available call our Lymphoma Nurses on 1800 953 081.