What is Hodgkin Lymphoma (HL)








HL is a type of cancer that makes some of your blood cells, called B-cell lymphocytes grow too much, and stop working properly. Lymphocytes are special cells, so small you need to look at them with a microscope. They are a type of blood cell, and their job is to fight germs that can make you sick. Some of them can even fight cancer.
Cancer means that the lymphocytes:
- grow when they are not supposed to
- don’t behave the way they should, and
- sometimes travel to parts of your body that they’re not meant to go.
What makes B-cell Lymphocytes special?
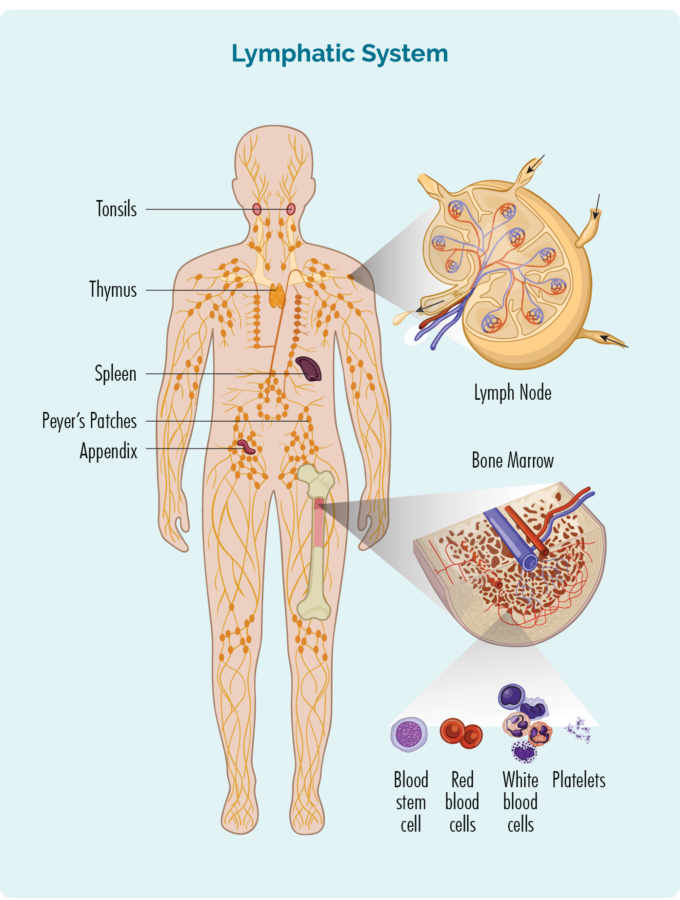
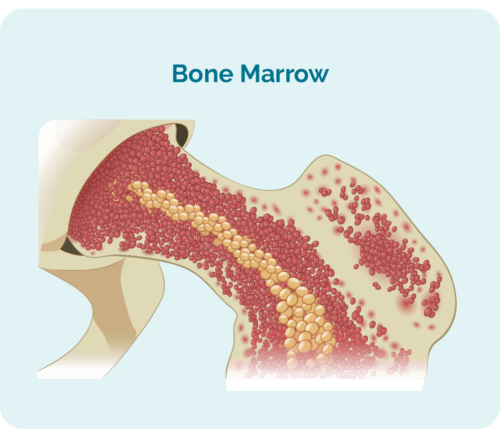
- they are made inside your bones in a place called “bone marrow”
- lymphocytes can travel to all parts of your body to fight infection, but usually live in your lymphatic system
- your lymphatic system includes some of your organs called spleen, thymus, tonsils and appendix as well as your lymph nodes that are found all over your body. Lymphatic vessels are like roads that connect all your lymphatic organs and lymph nodes together.
- lymphocytes help the neutrophils to fight germs.
- they also remember the germs so if they try to come back, your lymphocytes can get rid of them very quickly.
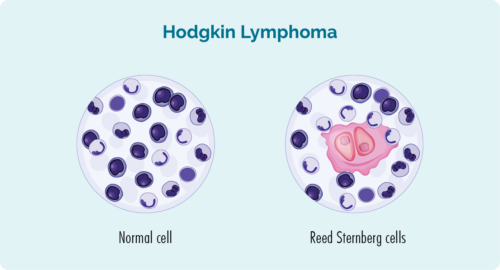
- when you have HL, your B-cell lymphocytes are called lymphoma cells and look different and are bigger than normal lymphocytes.
- the lymphoma cells are often also called Reed-Sternberg cells. (Reed and Sternberg were the names of the scientists who first identified these cells).
What does a Reed-Sternberg cell look like?
Here’s a picture to show you normal cells look like, and what Reed-Sternberg lymphoma cells look like.
Hodgkin lymphoma usually grows quickly, so it is sometimes called aggressive. But the good thing about aggressive Hodgkin lymphoma is that it often responds well to treatment, because the treatment is designed to attack the fast-growing cells.
For this reason, there is a very good chance you will be cured after treatment. That means you will no longer have cancer.
Symptoms of Hodgkin Lymphoma

The first symptom you might get if you have HL can be a lump, or several lumps that keep growing. These lumps can be on your neck, armpit, groin or abdomen (your tummy area). Lymph nodes in your abdomen may be harder to see and feel, because they are much deeper in your body than other lymph nodes.
The lumps are caused by your lymph nodes filling up with lymphoma cells, which makes them swell up. It usually is not painful but sometimes, if the swollen lymph nodes are putting pressure on other parts of your body it may cause some pain.
Where else can Hodgkin Lymphoma be found?
Sometimes, Hodgkin lymphoma can spread to other parts of your body such as your:
- lungs – your lungs help you breathe
- liver – your liver helps you to digest food, and cleans your body so you don’t build up harmful toxins (poisons) in your body
- bones
- bone marrow (this is in the middle of your bones and is where your blood cells are made).
- other organs that help your body work properly.
If your lymphoma cells spread to other areas of your body, it can be called advanced stage. We will talk about stages of HL more a little later.

Other symptoms you can get
- feeling really tired for no reason – often you still feel tired even after you’ve had a rest or a sleep
- feeling out of breath
- a dry cough that doesn’t go away
- bruising or bleeding more easily than usual
- Itchy skin
- blood in your poo or on the toilet paper when you go to the toilet
- infections that don’t go away, or keep coming back (recurrent)
- B-symptoms
Many of these signs and symptoms can be similar to other things such as infections. Usually with an infection or other cause the symptoms go away after a couple of weeks.
When you have HL though, the symptoms do not go away without treatment.
Your doctor may think you have an infection at first. But if they are concerned that it might be a type of lymphoma, they will order extra tests. If you’ve been to the doctor, and your symptoms are not getting better, you will need to go back to the doctor.
How is Hodgkin Lymphoma (HL) Diagnosed
There are many different types of lymphoma. They are usually grouped into Hodgkin lymphoma or non-Hodgkin lymphoma. Hodgkin lymphoma is then grouped into:
- Classical Hodgkin Lymphoma (cHL) or
- Nodular Lymphocyte Predominant Hodgkin Lymphoma (NLPHL)
Most of you will have cHL, with only 1 out of every 10 children and teenagers with HL having the NLPHL subtype.
How does my Doctor know what subtype I have?
It is important for your doctor to work out which one you have, because the types of treatment and medicines you get may be different to someone with a different subtype to you.
To find out what type of HL you have, your doctor will want to do some different tests. They will want to take samples of your swollen lymph nodes to test them and see what type of cells are in there. When the doctor takes a sample, it is called a biopsy. Depending on how old you are, and where your swollen lymph nodes are your, you might have your biopsy in the doctor’s room, in an operating room at the hospital or in a radiology department. Your doctor will you know where you and your parents/guardians need to go.
Biopsy
A biopsy can be done as an operation at the hospital. Your doctors and nurses will be very careful and make sure you are as comfortable as possible while they do the biopsy. You might even get some medicine that helps you to sleep during the biopsy, or make the spot they do the biopsy feel numb. This medicine is called an anaesthetic.
Once you have the biopsy, the sample will be taken to a laboratory where scientists will use different types of equipment like microscopes and special lights to look at the cells in the biopsy. By using these different types of equipment, they can see different parts of the lymphoma cells and help your doctor to diagnose what subtype of HL you have.
Some types of biopsies you might have include:
Core or fine needle biopsy
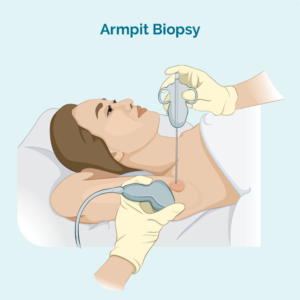
The doctor or nurse practitioner will put a needle into your swollen lymph node and remove a small sample of of the lymph node. You will have some medicine to numb the area so it doesn’t hurt, and depending on your age, you may even some medicine to make you sleepy so you can stay really still.
If the lymph node is deep inside your body and they can’t feel it, the doctor may use a ultrasound or specialised x-ray (imaging) guidance to help them see when they take the biopsy.
Excisional node biopsy
this may involve a more invasive day surgery to remove lymph nodes in other areas of your body that can’t be reached by a needle. This is usually done under general anaesthetic and you will have a small wound and stitches.
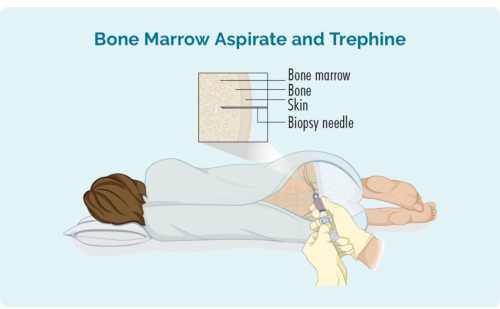
Bone marrow biopsy
A bone marrow biopsy involves the doctor placing a needle into your lower back and into your hip bone where your blood cells are made. There are two samples the doctor will take from this space including:
- Bone marrow aspirate (BMA): this test takes a small amount of the liquid found in the bone marrow space
- Bone marrow aspirate trephine (BMAT): this test takes a small sample of the bone marrow tissue
Waiting for results
It can take a couple of weeks to get your results back. Waiting for results can be a stressful time for you and your loved ones. It is important for you and your mob or family and friends to reach out and talk to someone you trust during this time. If you’re not sure who to talk to, or if you have questions, you can always call or email our lymphoma care nurses.
For details on how to contact them please click on the blue contact us button at the bottom of the screen.

Subtypes of Hodgkin Lymphoma
As we mentioned above, there are different types of HL – classical Hodgkin Lymphoma and Nodular Lymphocyte Predominant Hodgkin Lymphoma (NLPHL).
Classical Hodgkin Lymphoma is then further broken up into four other different types. These include:
- Nodular Sclerosis Classical Hodgkin Lymphoma (NS-cHL)
- Mixed cellularity classical childhood Hodgkin Lymphoma (MC-cHL)
- Lymphocyte-rich classical Hodgkin Lymphoma (LR-cHL)
- Lymphocyte-depleted classical Hodgkin Lymphoma (LD-cHL)
To learn more about these subtypes of HL, click on the headings below.
Classical Hodgkin Lymphoma Subtypes
NS-cHL is more common in older children and teenagers. Almost half of everyone with classical Hodgkin lymphoma will have this NS-cHL subtype.
Boys and girls can both get NS-cHL, but it is a little bit more common in girls.
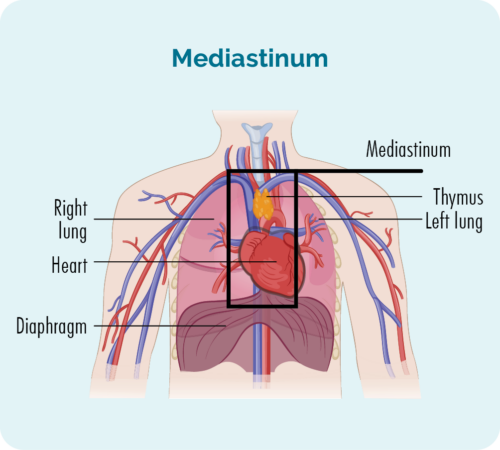
NS-cHL usually starts in lymph nodes deep inside your chest in an area called your mediastinum. You may or may not be able feel you swollen lymph nodes, but some other symptoms you may get with type of HL include:
- coughing
- pain or an uncomfortable feeling in your chest
- feeling short of breath
NS-cHL can also start, or spread to other parts of your body such as your spleen, lungs, liver, bone or bone marrow.
Mixed cellularity classical Hodgkin Lymphoma (MC-cHL) is more common in children less than 10 years of age. But it can still affect children and teenagers of any age. If you have MC-cHL, you may notice new lumps just under your skin. This is because the lymphoma cells gather and grow in your lymph nodes in the fatty tissue just under your skin. We all have this fatty tissue and it helps to protect our organs underneath, and keep us warm during cold weather. Some lymphoma cells might also be found in your other organs.
MC-cHL can sometimes be tricky for your doctor to diagnose because it looks like a different subtype of lymphoma called peripheral T-cell lymphoma. For this reason, your doctor may want to do extra tests to make sure you have MC-cHL so they can give you the right medicines.
Lymphocyte-rich classical Hodgkin lymphoma (LR-cHL) is a rare subtype of HL, so not many of you will have this subtype. But for those of your that do, it usually responds very well to your treatment. Most of you will be cured after your treatment. Most of you will notice some lumps just under your skin if you have LR-cHL because the lymphoma cells grow in the lymph nodes just under your skin.
LR-cHL can also be tricky for your doctor to diagnose because it sometimes look like a different type of HL called Nodular lymphocyte predominant Hodgkin Lymphoma (NLPHL). Both LR-cHL and NLPHL look the same, but different medicines are used to get rid of them.
Lymphocyte-depleted classical Hodgkin Lymphoma (LD0cHL) is probably the least common subtype of classical Hodgkin lymphoma in children and teenagers. It is more common if you have an infection called human immunodeficiency virus (HIV) or if you have ever had an infection called Epstein-Barr virus (EBV).
You may not have unusual lumps or swollen lymph nodes if you have LD-cHL because it often grown in the middle of your bones in a place called your bone marrow. This is the place where your blood cells are made. However, it can also start deep in your abdomen (or tummy) area, so the lumps may be too deep for you to feel.
Nodular Lymphocyte Predominant Hodgkin Lymphoma (NLPHL)
Nodular Lymphocyte Predominant Hodgkin Lymphoma (NLPHL) is a very rare subtype of HL, but it is more common in children younger than 10 years of age.
Your doctor can diagnose your with NLPHL if your cells look a certain way. It may seem funny, but we sometimes say the lymphoma cells in NLPHL look like popcorn. Take a look at the picture and you’ll see what we mean.

How is Nodular Lymphocyte Predominant Hodgkin Lymphoma (NLPHL) different to classical Hodgkin Lymphoma?
NLPHL grows more slowly than Classical Hodgkin Lymphoma. If you have NLPHL , you may be cured after treatment which means the lymphoma will go away and never come back. But, for some of you, it may come back. Sometimes it can come back quickly, and other times you might live without lymphoma for many years.
If your NLPHL comes back it is called a relapse. The only sign of a relapse might be a swollen lymph node that does not go away. This might be in your neck, armpit, groin or other area of your body. If you get other symptoms, they will be similar to the symptoms we listed above.
Staging and Grading of Hodgkin Lymphoma (HL)
Once your doctor has diagnosed you with HL, they will want to do more tests to see how many parts of your body have lymphoma cells, and how fast they are growing.
Staging looks at where the HL is. Remember earlier we talked about your lymphocytes. We found out that although they are made in your bone marrow and live in your lymphatic system, they can also travel to any part of your body. Because the cells of your lymphoma are cancerous lymphocytes, the HL can also be in your bone marrow, lymphatic system or any other part of your body.
Staging Tests and Scans
So, your doctor will order some scans to take pictures of the inside of your body to see where these HL cells are hiding. These scans might include:
CT scan (this stands for computed tomography scan)
This is like a special X-ray that gives a detailed picture of everything inside your chest, abdomen (tummy area) and pelvis (near your hip bones). Your doctor will be able to see any swollen lymph nodes or tumours in these areas on this scan.
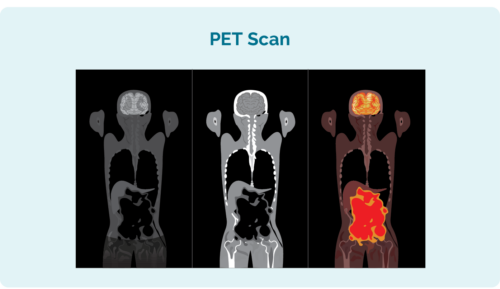
PET scan (this stands for Positron Emission Tomography scan)
This scan looks inside your whole body. The areas that have lymphoma look brighter than other area. You will need to have needle in your hand or arm for this one because they will inject some fluid that helps the lymphoma cells light up on the computer image. The nurses are very good at doing this and will take special care to make sure it doesn’t hurt too much.
MRI scan (This stands for Magnetic Resonance Imaging)
This scan uses magnets inside a machine to take pictures of the inside of your body. It doesn’t hurt, but because there are magnets swirling around in the machine it can be very noisy. Some people don’t like these noises so you might have some medicine to make you a little sleepy during the scan, so it doesn’t worry you.
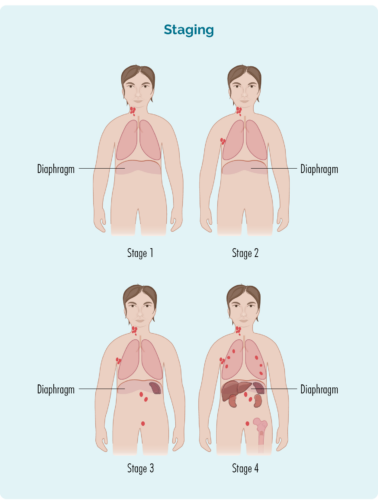
How is my HL stage numbered?
Staging is numbered from the number one to the number four. If you have stage one or two you will have an early-stage HL. If you have stage three or four, you will have an advanced stage HL.
Advanced stage HL can sound scary. But, because your lymphocytes travel all around your body, lymphoma is considered a “systemic” disease. So, advanced lymphomas including HL are very different to other cancers with advanced disease. Many solid tumours, such as tumours in the brain, breast, kidneys and other places cannot be cured if they are advanced.
But many advanced stage lymphomas can be cured with the right treatment, and this is often the case for children and teenagers with HL.
This picture is a good example of how the different stages might look. The red parts show where the lymphoma might be in each stage – yours may be a little different, but will follow roughly the same pattern.
stage 1 | Your HL is in one lymph node area, either above or below your diaphragm* |
stage 2 | Your HL is in two or more lymph node areas, but on the same side of your diaphragm* |
stage 3 | Your HL is in at least one lymph node area above and at least one lymph node area below your diaphragm* |
stage 4 | Your HL is in multiple lymph nodes areas, and has spread to other parts of your body, such as your bones, lungs, or liver |
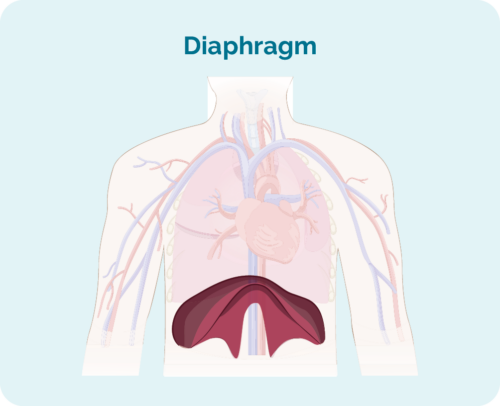
What is your diaphragm?
Your diaphragm is a dome shaped muscle that separates the organs in your chest, form the organs in your abdoment. It also helps you to breathe by helping your lungs move up and down.
Other important things to know about your stage
As well as a staging number, you might be given a letter after the number.
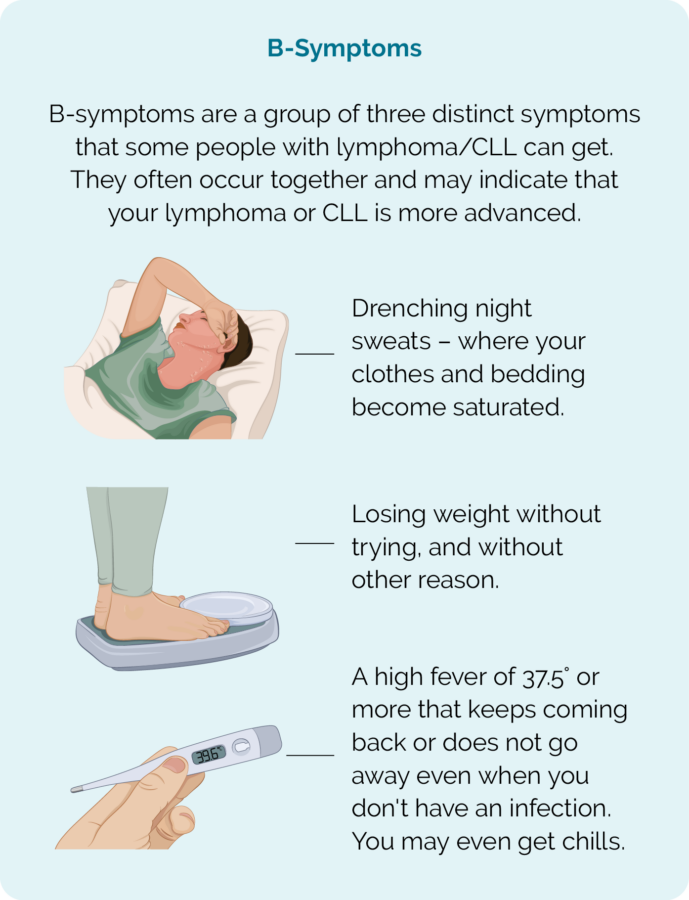
Do you remember what we said earlier about the B-symptoms? They are a group of symptoms that can happen together when you have lymphoma. They include:
- Drenching night sweats that wet your clothes and bedding
- Fevers and chills
- Losing weight without trying
If you have these B-symptoms you will have a “B” after your staging number, but if you don’t have B-symptoms you will have an “A” after your staging number.
If one of your organs, such as your lungs, liver or bones have HL you will have the letter “E” after your staging number.
If you have a lymph node or tumour that is more than 10cm in size it is considered a bulky disease. If you have bulky disease, you will have the letter “X” after your staging number
Finally, if your spleen has HL in it, you will have the letter “S” after your staging number. Your spleen helps to keep your blood clean, and is a major organ of your immune system. It is where a lot of your white blood cells live and where your B-cell lymphocytes make a lot of antibodies to fight germs.
See what these different things can mean in the table below.
Meaning | Importance |
|
|
|
|
|
|
Grading helps your doctor make good choices about the treatments they offer you.
Just like staging, your grade will be given as a number from one to four. It might be written as G1, G2, G3 or G4. When your lymphocytes become cancerous, they begin to look different to your normal lymphocytes. If you have a low grade lymphoma such as G1, the cells might be growing slowly and only be a little different to your normal lymphocytes, but with a higher grade, they grow very fast and can look nothing like your normal cells. The more different they look, the less they are able to work properly.
As we mentioned earlier, you will have biopsies of your swollen lymph nodes or tumour. As well as the biopsies mentioned above, you will have blood tests and you may also have another type of biopsy called a bone marrow biopsy.
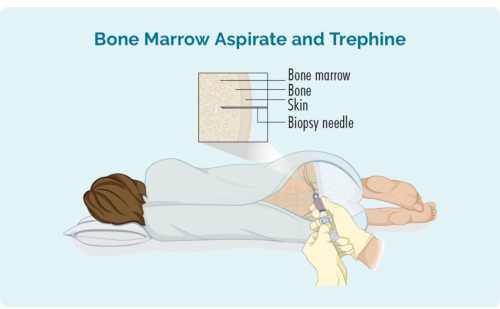 Bone marrow biopsies are where the doctor puts a needle into your back and into your hip bone to take out some of the bone marrow to send to pathology for testing. This might sound awful, but you will be given a local anaesthetic to the area to make it numb, and you might even be given medicine to make you sleepy so you don’t feel or remember having the bone marrow biopsy done.
Bone marrow biopsies are where the doctor puts a needle into your back and into your hip bone to take out some of the bone marrow to send to pathology for testing. This might sound awful, but you will be given a local anaesthetic to the area to make it numb, and you might even be given medicine to make you sleepy so you don’t feel or remember having the bone marrow biopsy done.
Here is on overview of each grade:
- G1 – low grade – your cells look close to normal and they grow and spread slowly.
- G2 – intermediate grade – your cells are starting to look different but some normal cells exist and they grow and spread at a moderate rate.
- G3 – high grade – your child’s/ your cells look fairly different with a few normal cells and they grow and spread faster.
- G4 – high grade – your child’s/ your cells look most different to normal and they grow and spread the fastest
Other Tests
You may have other tests before you start treatment, and during treatment to make sure your body is able to cope with the medicines you will have. These can include:
- Regular blood tests
- Ultrasounds or other scans and tests of some of your organs including your heart, lungs and kidneys
- Cytogenetic tests – these are special tests to see if there are any changes in your genes. Your genes tell the cells in your body how to grow and how to work. If there is a change (also called a mutation or a variation) in your genes, they can give the wrong instructions. These wrong instructions can cause cancer – such as HL to grow. Not everyone will need this test though.
- Lumbar puncture – This is a procedure where the doctor puts a needle into your back near your spine and takes out some fluid. This will only happen if he things there is a chance your HL is in your brain or spine, or is likely to spread there. Some children or teenagers may have some sedation to make you sleepy during this sleepy so it doesn’t hurt, and to make sure you keep still during the procedure.
Questions for your doctor before you start treatment
Once your doctor has collected all the information from your biopsies, scans and other tests; they will be able to put a plan together to manage your treatment and keep you safe. Sometimes doctors will talk to other doctors or other specialists to make sure that they make the best plan possible for you. When these specialists get together to make a plan, it is called a multidisciplinary team meeting – or an MDT meeting.
We will talk about the types of treatments you might get a little further down this page. But first it is important that you feel comfortable to ask your doctor any questions you have before you start treatment. This will help you to know what to expect, and to feel more confident.
It can be hard knowing what the right questions are to ask. But to be honest, there are no right or wrong questions. Everyone is different and the questions you have may different to the questions another child or teenager has. What’s most important is that there are no silly questions when it comes to your health and treatment. So feel confident to ask about anything that‘s on your mind.
Some Questions to get you started
To help get you started we have listed some questions below that you or your parents might like to ask. If you’re not ready, or forget to ask the questions before treatment, that’s ok, you can ask the doctor or your nurse anytime. But knowing the answers before you start treatment, might help you feel more confident.
Questions for your doctor before you start treatment | Additional Questions if you live in rural Australia |
|
*If your doctor recommends having radiation treatment you will need to go to appointment every day. If You need help with a place to stay during treatment, please talk to your doctor or nurse about what help is available to you. You can also contact the Cancer Council or Leukemia Foundation in your state and see if they can help with somewhere to stay. |
Some additional questions your parents might like to ask
- What do I need to tell my child’s teachers about treatment and missing school terms? What tutoring or catch-up services are available and how do I access them?
- What financial, accommodation and travel assistance is available to us during my child’s treatment?
- Is there a social worker who can help us arrange these things?
- What extra support is available for my other children while their brother/sister is having treatment?
- What changes do we need to make at home to keep my child safe during treatment?
- What things do I need to look out for while my child is having treatment, and after their treatment?
- Will my child still be able to have children when they are older – what can be done to protect their fertility?
Treatment for Hodgkin Lymphoma
Your health care team will consider many things about you before making a final decision on what they think is the best treatment for you. Some of the things they will consider include:
- Whether you have a classical subtype of HL or Nodular Lymphocyte Predominant Hodgkin Lymphoma (NLPHL)
- How old you are
- If you have any other illnesses or disabilities
- If you have any allergies
- How well you are feeling both physically (your body) and mentally (your mood and thoughts).
Your doctor or nurse can explain your treatment plan and the possible side-effects to you. Side-effects are things that can happen because of your treatment, such as feeling sick, or your hair falling out or many other things. If you have side-effects, it’s important to let your nurse or doctor know so they can help you feel better.
If there is anything you don’t understand, or you are feeling worried, talk to your doctor or nurse and ask them to explain things to you.
You can also phone or email the Lymphoma Australia Nurse Helpline with your questions. we can help you to get the right information. Just click on the Contact us button on the bottom of this screen.
There are different types of treatment. You may have one type, of several types depending on your situation. These include:
Supportive Care
Supportive care is given to help you feel better during treatment, and get well faster.
For some of you, your lymphoma cells may grow too fast and too big. This makes your bone marrow, bloodstream, lymph nodes, liver or spleen too crowded. Because of this, you may not have enough healthy blood cells. Supportive treatment can include giving you a blood or platelet transfusion to make sure you have enough healthy blood cells.
If you have an infection, you may have antibiotics to help you get better quicker. In some cases you might even have a medicine called GCSF to help your body make more white blood cells to fight infection.
Supportive treatment can also include bringing in another team called the palliative care team. The palliative care team are great at making sure you are comfortable, and improving your symptoms or side effects. Some of the things they can help you with include pain, feeling sick or feeling worried or anxious. They can also help plan how to manage your health care in the future.
It’s a good idea to ask your doctor or nurse what supportive treatments might be good for you.
Radiation treatment (Radiotherapy)
Radiotherapy uses radiation to kill cancer cells. It is like high-energy X-rays and is performed every day, usually from Monday to Friday for several weeks. It is can be used to cure cancer, to help put you into remission – where the cancer is no longer detectable (but may come later), or it can be used to manage some symptoms.
Some symptoms that may be treated with radiotherapy include pain or weakness. This can happen if your lymphoma is putting pressure on your nerves or other parts of your body. The radiotherapy makes the lymphoma (tumour) smaller so it doesn’t keep putting pressure on your nerves or parts of your body it is causing pain in.
Chemotherapy (chemo)
You might have chemo as a tablet and/ or have it as a drip (infusion) into your vein (into your bloodstream) at a cancer clinic or hospital. You may have more than one type of chemo, and it may be combined with a monoclonal antibody or immune checkpoint inhibitor. Chemo kills fast growing cells, so it can also affect some of your good cells that grow fast causing side effects.
Monoclonal Antibody (MAB)
You may have a MAB infusion at a cancer clinic or hospital. MABs attach to the lymphoma cell and attract other diseases fighting white blood cells and proteins to the cancer so your own immune system can fight the HL. In some cases, the MAB may be joined to another toxin that directly kills the cancerous lymphoma cells. These MABs are called conjugated MABS.
Immune checkpoint inhibitors (ICIs)
ICIs are given as an infusion and work to improve your own immune system, so that your own body can fight your cancer. They do this by blocking some of the protective barriers lymphoma cells put up, that make them invisible to your immune system. Once the barriers are removed, your immune system can see and fight the cancer.
Targeted therapy
You may take these as a tablet or infusion into your vein. Oral therapies may be taken at home, though some will require a short hospital stay. If you have an infusion, you may have it at a day clinic or in a hospital. Targeted therapies attach to the lymphoma cell and block signals it needs to grow and produce more cells. This stops the cancer from growing and causes the lymphoma cells to die off.
Stem-cell transplant (SCT)
If you are young and have aggressive (fast growing) HL a SCT may be used. Stem cells help to replace your bad cells with good, healthy stem cells that can grow into any type of blood cell you need.
CAR T-cell Therapy
To learn more about CAR T-cell therapy, please see our webpage Chimeric antigen receptor (CAR) T-cell therapy.
Parents and older children – If you would like more information on these treatments, please see our webpage on Treatments here.
First-Line Treatment
Starting Treatment for Hodgkin Lymphoma (HL)
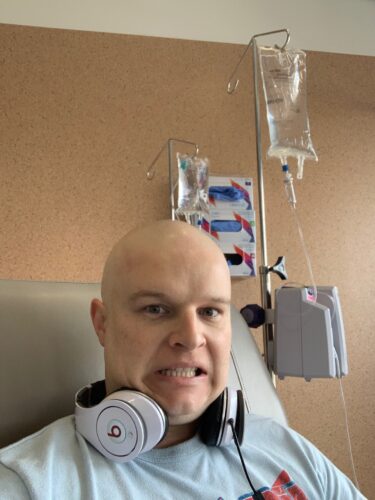
When you first start treatment, you might feel a bit like the man in this photo. But knowing what to expect can make it a little easier. So keep reading and let us tell you about what might happen.
The first time you have a type of treatment it is called first-line treatment. When you start treatment, you will have it in cycles. That means you will have the treatment, then a break, then another round (cycle) of treatment.
It’ss usually given as an infusion into your vein. Most children and teenagers will need to have a device called a tunnelled catheter that the medicine is put through. The tunnelled catheter is used so you won’t need to have a needle every time you have treatment or a blood test. You can find information on tunnelled catheters by clicking on the button below.
To see more about the types of first-line treatment you might have, please click on the banner depending on whether you have Nodular Lymphocyte Predominant Hodgkin Lymphoma (NLPHL), or classical Hodgkin lymphoma. Remember that classical Hodgkin Lymphoma includes:
- Nodular sclerosis classical Hodgkin lymphoma (NS-cHL)
- Mixed cellularity classical Hodgkin lymphoma (MC- cHL)
- Lymphocyte-rich classical Hodgkin lymphoma (LR-cHL)
- Lymphocyte-depleted classical Hodgkin lymphoma (LD- cHL)
The treatment for Nodular Lymphocyte Predominant Hodgkin lymphoma (NLPHL) is very different to classical Hodgkin lymphoma (cHL). If you have an early stage NLPHL your treatment may include one or more of the following:
- Watch and wait active monitoring until symptoms need to be treated.
- Radiotherapy only.
- Surgery, if the tumour can be completely removed.
- Combination chemotherapy with or without low-dose external beam radiotherapy. Chemotherapy may include medicines called:
- AVPC (doxorubicin, vincristine, cyclophosphamide and steroid called prednisone)
- CVP (cyclophosphamide, vincristine and a steroid called prednisone)
- COG-ABVE-PC (doxorubicin, bleomycin, vincristine, etoposide, cyclophosphamide and a steroid called prednisone).
- Rituximab – this medicine is administered intravenously. It is a monoclonal antibody which targets a receptor called CD20 on B-cells, and has worked very well to treat other types of B-cell lymphoma.
- Clinical trial participation – where you might get to try new or different types of medicine or treatments.
Classical Hodgkin lymphoma (cHL) is a rapidly growing lymphoma, so treatment needs to start soon after you are diagnosed. The standard treatment for children and teenagers with cHL is a combination of chemotherapy. Some children and teenagers also receive radiotherapy to specific areas of lymphoma after chemotherapy.
The doctor may recommend one of the following first-line treatments for childhood classical Hodgkin lymphoma:
COG-ABVE-PC
This protocol includes a steroid called prednisolone and chemotherapy medications called
- doxorubicin
- bleomycin
- vincristine
- etoposide
- cyclophosphamide
You will have this every 21 days (3-weeks) for 4-6 cycles.
Bv-AVECP
This protocol includes the steroid prednisolone, and a conjugated MAB called brentuximab vedotin and the chemotherapy medications called:
- Doxorubicin
- Vincristine
- Etoposide
- cyclophosphamide
In some cases, if you are 15 years or older you may have your treatment at an adult hospital. If you do, the treatment protocol may be different. For more information on treatments you may get if you are at an adult hospital, please see our adult HL page. The link to the adults HL page is at the top of this page.
Second-Line and ongoing treatment for Hodgkin Lymphoma (HL)
After treatment most of you will go into remission. Remission is a period of time where you have no signs of HL left in your body, or when the HL is under control and doesn’t require treatment. This time can last for many years, but rarely, your HL can relapse (come back). When this happens, your doctor might want to give you another treatment.
In some cases, you may not go into remission with your first-line treatment. If this happens, your HL is called “refractory”. If you have refractory HL your doctor will probably want to try a different medication. Your HL may also be called refractory if you have treatment and go into remission, but the remission lasts for less than 6 months.
Treatment for Refractory and Relapsed Hodgkin Lymphoma (HL)
Treatment you have if you have refractory HL or after a relapse is called second-line therapy. The goal of second-line treatment is to put you into remission again, or for the first time and can be very effective.
If you have further remission, then relapse and have more treatment, these next treatments are called third-line treatment, fourth-line treatment and such.
You may need several types of treatment for your HL. Experts are discovering new and more effective treatments that are increasing the length of remissions and helping to keep you healthier during and after treatment.
How will the doctor choose the best treatment for me?
At the time of relapse, the choice of treatment will depend on several factors including.
- How long you were in remission for
- Your general health and age
- What HL treatment/s you have received in the past
- Your preferences.
Your doctor will be able to talk to you and your parents or guardians about the best second-line treatment for you.
