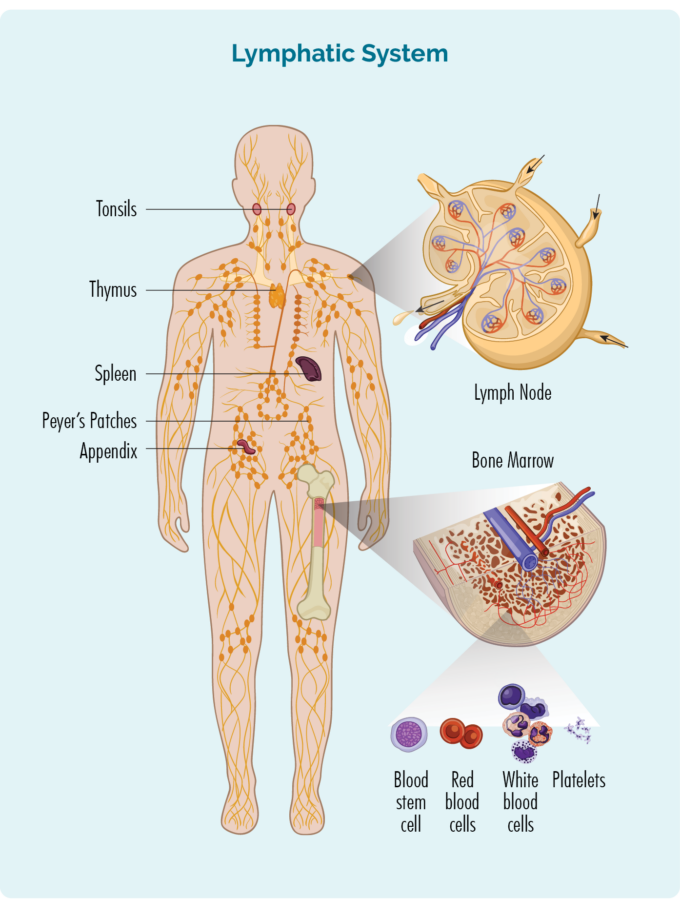
To understand Marginal Zone Lymphoma (MZL) you need to know a bit about your B-Cells
B-Cells:
- Are a type of white blood cell
- Fight infection and disease to keep you healthy.
- Remember infections you had in the past, so if you get the same infection again, your body’s immune system can fight more effectively and quickly.
- Can travel through your lymphatic system, to any part of your body to fight infection or disease.
- Are made in your bone marrow (the spongy part in the middle of your bones), but usually live in your lymphatic system which includes your:
- lymph nodes
- lymphatic vessels and lymph fluid
- organs – spleen, thymus, tonsils, appendix and patches of immune cells in areas lining parts of your body (e.g., peyers patches in your bowels).
When you have MZL the cancerous B-cells:
- Grow uncontrollably.
- Will not work as well to fight infections and disease.
- Can become larger than they should and can look different to healthy B-cells.
- Can cause lymphoma to develop and grow in any part of your body.
Marginal Zone Lymphoma (MZL) subtypes - Overview
Subtypes of MZL are all very unique and each is diagnosed and treated quite differently. Click on the subheadings below to see an overview of the three subtypes.
Mucosa-associated lymphoid tissue (MALT) Marginal Zone Lymphoma (MZL)
MALT MZL is known as an extra-nodal lymphoma because it starts in the marginal zone of your lymphoid tissue, but not in your lymph nodes.
It is the most common form of MZL, with around 6 out of 10 people (60%) with MZL having a MALT subtype. You can get it at any age, but it usually develops when you’re in your 60’s.
- Mucosa is the soft, moist, protective layer of cells that lines many parts of your body, such as your mouth, gut, airways and some internal organs.
- Lymphoid tissue is an area in your body or some organs where lymphocytes live – such as Peyer’s patches in your bowels.
- Mucosa-associated lymphoid tissue (MALT) are groups of lymphocytes in your mucosa that help protect you from infections.
- MALT includes your tonsils at the back of your throat, as well as lymphoid tissue that may be scattered around the rest of your body, such as your gut, lungs, skin, thyroid gland and salivary glands.
MALT Marginal Zone Lymphoma (MZL) subtypes
MALT Marginal Zone Lymphoma (MZL) can form if abnormal B-lymphocytes collect in your lymphoid tissues. MALT MZL is further grouped into:
- Gastric MALT MZL, which develops in your stomach. This is the most common subtype of MALT MZL.
- Non-gastric MALT MZL, which develops in lymphoid tissue outside of your stomach. It is most common in your eyes (ocular adnexa), followed by lung and salivary gland. It can also occur in your skin, thyroid or other parts of your gut or bowel.
It is important to know if you have gastric or non-gastric MALT because they are treated differently. If you’re not sure what type of MALT Marginal Zone Lymphoma (MZL) you have, please ask your doctor or treating team to explain this to you.
Risk factors for developing MALT Marginal Zone Lymphoma (MZL)
MALT MZL is more common in people with long term (chronic) inflammation from an infection or autoimmune disorder. It’s important to know though, that most people with these risk factors will not develop MZL.
Table 1 below lists the infections and autoimmune disorders that may cause MALT MZL.
Table 1
Sites of MALT lymphoma | Possible Cause (or risk factors) |
Gastric MALT lymphoma | Helicobacter pylori (H. pylori), is a type of bacteria that causes stomach ulcers. It contributes to most cases of gastric MALT MZL. Treatment for gastric MALT MZL focuses on curing the H. pylori infection. |
Tear ducts and tissue around the eye (non-Gastric) | Chlamydophila psittaci (C Psittaci) is an infection linked to MALT of the tear ducts and eye tissue. This is spread by birds and can cause lung infections. |
Skin (non-Gastric) | Borrelia burgdorferi is an infection that may be linked to MALT MZL of the skin. It is spread by ticks and causes LYME disease. |
Small bowel (non-Gastric) | Campylobacter jejuni is an infection that may be linked to MALT MZL of the small bowel. It is a common cause of food poisoning. |
Lungs (non-Gastric) | Achromobacter xylosoxidans is an infection that may be linked to MALT MZL of the lungs. It can cause blood or lung infections mostly in people with lowered immune systems. |
Salivary glands (non-Gastric) | Sjogren’s syndrome is a disorder or your immune system which may be linked to MALT MZL of the salivary glands. |
Thyroid gland (non-Gastric) | Hashimoto’s thyroiditis is a disorder of the immune system that may be linked to MALT MZL of the thyroid gland |
 Nodal MZL is named nodal, because it starts in the marginal zone of your lymph nodes. It is the rarest subtype of MZL affecting only 1 in every 10 people with MZL. It is most common in people over the age of 50 years, however there is rare paediatric type that can affect children.
Nodal MZL is named nodal, because it starts in the marginal zone of your lymph nodes. It is the rarest subtype of MZL affecting only 1 in every 10 people with MZL. It is most common in people over the age of 50 years, however there is rare paediatric type that can affect children.
Many subtypes of lymphoma begin in the lymph nodes, so it can be difficult at first to get an accurate diagnosis of your subtype.
Little is known about the causes of Nodal MZL. However, it is thought people who have an underlying autoimmune disease, or who have had a viral infection in their liver, called Hepatitis C (Hep C) are more likely to develop to it.
Nodal MZL often responds well to treatment, but as with most indolent lymphomas, it often comes back. This is called a relapse. It is not uncommon to need treatment more that once for your Nodal MZL, but it usually responds well to treatment and is kept under good control.
Splenic MZL is a rare subtype that starts in your spleen and can include your blood and bone marrow. Your spleen is a lymphatic organ that sits just under your diaphragm. It is an organ of your lymphatic system and is where many of your B-cell lymphocytes live, and produce antibodies. Your spleen also helps to filter your blood, breaking down old red cells to make way for new health cells and storing white blood cells and platelets, which help your blood to clot. You can see the location of your spleen in the picture of the lymphatic system at the top of this page.
Splenic MZL affects adults most commonly around the age of 65 years. It is more common in people who have an autoimmune disorder or who have had Hepatitis C – a viral infection affecting your liver. However, not all people with splenic MZL will have these risk factors.
General symptoms of Marginal Zone Lymphoma (MZL)
MZL is usually a slow growing (indolent) lymphoma, so you may not have any symptoms in the early stages of your disease. Some symptoms you do have will be dependant on the subtype of MZL you have and is covered under the subtypes below.
However, there are some symptoms that can affect anyone with lymphoma.
Symptoms you may get
If you do experience symptoms they may include:
- swollen lymph nodes – a lump that you can see or feel
- feeling unusually tired (fatigued)
- feeling out of breath
- bruising or bleeding more easily than usual
- infections that don’t go away, or keep coming back (recurrent)
- sweating at night more than usual
- losing your appetite (not wanting to eat)
- losing weight without trying
- itchy skin
- B-symptoms.
Subtype Specific Symptoms of Marginal Zone Lymphoma (MZL)
The symptoms you may get with MALT MZL will depend on where your lymphoma is.
Gastric MALT Marginal Zone Lymphoma (MZL)
Symptoms are related to your stomach and can include:
- Persistent indigestion (often this the only symptom)
- Stomach pain
- Nausea (feeling sick and like you are going to vomit)
- Vomiting
- Weight loss (unintentional)
- Some people may have symptoms of anaemia (tiredness or short of breath) caused by bleeding in the stomach
Non-gastric MALT Marginal Zone Lymphoma (MZL)
You may not get any symptoms. Non-gastric MALT MZL is often diagnosed accidentally when your doctors are doing tests for something else. Symptoms are varied and depend on which part of your body is affected. Some of you (around half) can have MALT lymphoma in more than one area of your body. This can create a mixture of symptoms. It is important to tell your doctor about all your symptoms, as it can help them choose the best treatment option for you, and when to begin treatment.
Table 2
Extra nodal MALT lymphoma location | Common symptoms |
Stomach or bowel |
|
Tear ducts or tissues around the eye | Symptoms usually only affect one eye but rarely, both eyes may be affected.
|
Lungs | Often you will have no or few symptoms but you may have cough, shortness of breath, coughing up blood or chest pain. |
Salivary glands |
|
Skin | Skin changes can develop in one place, or in several places around your body. It usually shows up on your arms, chest or back as pink, red or purple patches or lumps. These changes happen over a long period of time, so may not be very noticeable. |
Thyroid gland | You may notice a lump (swollen lymph node) on the front of your neck or have a hoarse voice. You can also get shortness of breath and have trouble swallowing (dysphagia). If your thyroid gland is underactive, you may:
|
 Nodal MZL usually starts in your lymph nodes in your head and neck, but can occur in other areas of your body too. This can cause a lump/s to be seen or felt as your lymph nodes become full of cancerous lymphoma cells, causing them to swell. As the disease becomes more advanced it can spread to other parts of your body.
Nodal MZL usually starts in your lymph nodes in your head and neck, but can occur in other areas of your body too. This can cause a lump/s to be seen or felt as your lymph nodes become full of cancerous lymphoma cells, causing them to swell. As the disease becomes more advanced it can spread to other parts of your body.
Symptoms of Nodal MZL are usually related to the swelling of your lymph nodes. Therefore, symptoms can vary depending on where your lymphoma is, but can include:
- Lymph nodes in or near your neck may put pressure on your airways or your oesophagus (the pipe food travels from your mouth to stomach). These may cause difficulty breathing or eating as they become bigger.
- Lymph nodes near your nerves may cause pain as the lymph nodes press on them.
- As your lymphoma grows and takes up more of your body’s energy you may experience B-symptoms.
The most common symptom of splenic MZL is an enlarged spleen.
Usually your spleen cannot be felt, but if it is enlarged, your doctor may be able to feel it under your ribs. When your spleen gets too big, it can put pressure on your stomach making you feel full, even if you haven’t eaten much. You may also have pain or discomfort in your abdomen (tummy).
As your lymphoma progresses you may get a build up of lymphoma cells in your bone marrow. This, along with having too many lymphoma cells in your spleen can prevent your body from being able to make new blood cells. Your body’s ability to store your blood cells for later use, can also be decreased. This means you may get symptoms that relate to low blood.
Low Blood counts
- Low white blood cells – Your white blood cells, including your lymphocytes fight infection and protect you from disease. Low white blood cells can result in infections that are difficult to get rid of or keep coming back
- Low platelets – Platelets help clot your blood to stop you from bleeding or bruising too much, so you may notice you bleed or bruise more easily.
- Low red blood cells – your red blood cells carry oxygen around your body on a protein called haemoglobin. If your red blood cells are low you may experience:
- shortness of breath
- fatigue – which is extreme tiredness not improved with rest or sleep
- dizziness
- confusion or difficulty concentrating
- look more pale than usual.
Abnormal Proteins
Some people with splenic Marginal Zone Lymphoma (MZL) may also produce abnormal proteins called cryoglobulins. These proteins clump together when you get cold, leading to:
- poor circulation – you may notice your fingers and toe turn blue or you may have numbness or tingling in them
- headaches
- confusion
- nosebleeds
- blurred vision.
Diagnosis - How is Marginal Zone Lymphoma (MZL) diagnosed
Diagnosing MZL can take several weeks, or sometimes longer.
If your doctor thinks that you have lymphoma, they will need to organise a number of important tests. These tests are needed to either confirm or rule out lymphoma as the cause for your symptoms.
There are several different subtypes of MZL, so you may have extra tests to find out which one you have. This is important because the management and treatment of your subtype may be different to other subtypes of MZL.
You will need one or more biopsies. A biopsy is a procedure to remove part, or all of an affected lymph node and/ or a bone marrow sample. The biopsy is checked by scientists in a laboratory to see if there are changes that help the doctor diagnose MZL. Types of biopsies include:
Core or fine needle biopsy
This involves inserting a needle into a lymph node or lump and removing a sample of tissue. It is usually done with local anaesthetic, while you are awake.
If the affected lymph node is deep inside your body the biopsy may be done with the help of ultrasound or specialised x-ray guidance. You will need a general anaesthetic for this, and you will have a few stitches afterwards.
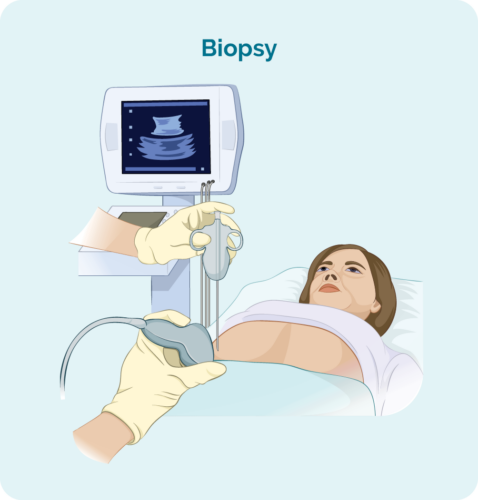
Excisional node biopsy
This may involve a more invasive day surgery to remove lymph nodes in other areas of your body that can’t be reached by a needle. It is usually done under general anaesthetic, and you will have a small wound and stitches.
Your doctor will choose the best biopsy for you.
You will also have blood tests so the doctor can get better understanding of your overall health.
Waiting for Results
Expect to wait several weeks to have all your tests and get the results back. This waiting time can be difficult, but it may help to know that with MZL being an indolent lymphoma, any delays in treatment during this time will not cause you any harm.
Let your doctor know if you are experiencing new symptoms, or they are getting worse during this time. Your treating team will be able to offer you advice on how best to manage your symptoms while waiting for results.
It can help to have someone to talk to during this time. If you have a family member or friend you can reach out to, let them know what’s going on and what you need from them. People often want to help, but don’t quite know what to do, or don’t want to impose. Letting them know what you need helps them and you.
Contact us
You can also contact our Nurse Hotline to talk to one of our Lymphoma Care Nurses. Just click on the Contact us button at the bottom of this page. We can help by sending you information or letting you know what support is available. You may also like to join one of our social media pages to chat with other people living with lymphoma.
Find us on our socials
Depending on what subtype your doctor suspects you have, you may need different diagnostic tests. Click on the headings below to learn about the diagnostic tests for each subtype.
MALT MZL is often associated with an infection, so your doctor may want to take a biopsy from the area if they suspect you have an infection. This means different types of procedures may be used to take the biopsy such as:
Gastroscopy and biopsy: A biopsy of your stomach. This involves placing a thin tube with a camera on it, through your mouth and down your digestive tract and into your stomach. Gastroscopy is usually done as a day procedure.
Bronchoscopy and biopsy: A biopsy of your lungs. With this procedure a thin tube with a camera on the end is placed down into your lung. This allows the doctors to get a closer look at the tissue in your airways and lungs, and take samples. In most cases, this is a same day procedure.
Breath test: Looks for certain gases that can be caused by different bacteria such as H. Pylori. You will be given a medication and after a short wait, you will be asked to breathe into a small balloon shaped bag. Your sample is then checked for gases which may confirm an infection.
Faeces test: You will collect a faecal (poo) sample and it will be sent to the pathology to test for the H. Pylori infection.
No additional tests for diagnosis.
In addition to the above tests, you may also have bone marrow biopsy to help diagnose splenic MZL. This is because another type of blood cancer called Waldenstrom’s Macroglobulinemia has very similar symptoms.
The bone marrow will provde information to help confirm that your lymphoma is Splenic MZL rather than Waldenstroms Macroglobulinemia. It will also show if it is has spread to your bone marrow. Bone marrow biopsies are described below under the section “What does staging mean”.
Staging and Grading Marginal Zone Lymphoma (MZL)
Once you have been diagnosed with MZL, your doctor will have more questions about your lymphoma. These will include:
- What stage is your MZL?
- What grade is your MZL?
Click on the headings below to learn more about staging and grading.
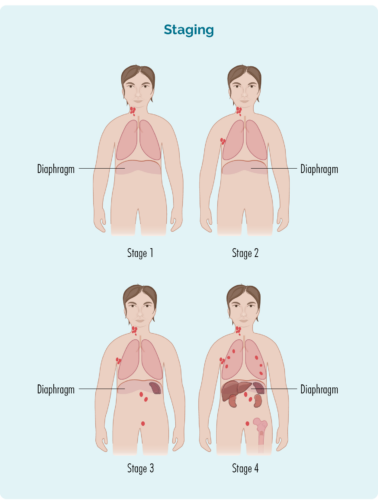
Staging refers to how much of your body is affected by your MZL or, how far it has spread from where it first started.
B-cells can travel to any part of your body. This means that lymphoma cells (the cancerous B-cells), can also travel to any part of your body. You will need to have more tests done to find this information. These tests are called staging tests and when you get results, you will find out if you have stage 1 (I), stage 2 (II), stage 3 (III) or stage 4 (IV).
Staging your Marginal Zone Lymphoma (MZL)
Your stage will depend on: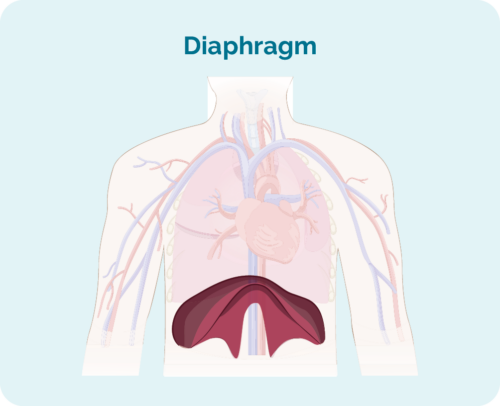
- How many areas of your body have lymphoma
- Where the lymphoma is – if it is above, below, or on both sides of your diaphragm
- Whether the lymphoma has spread to your bone marrow or other organs, such as your liver, lungs, skin or bone.
*Your diaphragm is a dome shaped muscle that separates your chest and your abdomen.
Stage 1 | one lymph node area is affected, either above OR below your diaphragm* |
stage 2 | two or more lymph node areas are affected on the same side of your diaphragm* |
stage 3 | at least one lymph node area above and at least one lymph node area below your diaphragm* are affected |
stage 4 | lymphoma is in multiple lymph nodes and has spread to other parts of your body (e.g., bones, lungs, liver) |
Extra information about your stage
Your doctor may also talk about your stage using a letter, such as A, B, E, X or S. These letters give more information about the symptoms you have, or how your body is being affected by the MZL. All this information helps your doctor find the best treatment plan for you.
Letter | Meaning | Importance |
A or B |
|
|
E & X |
|
|
S |
|
|
Staging Tests
To find out what stage you have, you may be asked to have some of the following staging tests:
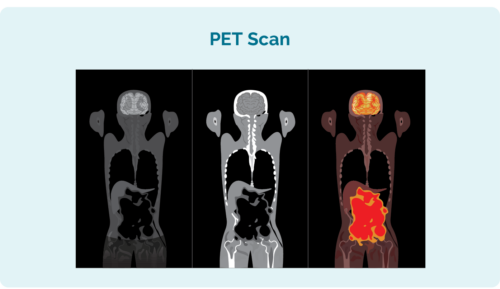
- Computed tomography (CT) scan – a scan of the inside of your chest, abdomen or pelvis.
- Positron emission tomography (PET) scan – this is a scan of your whole body. It involves a small needle to inject a fluid that makes lymphoma cells glow on the picture (or look “hot”). This helps the scan to pick up the location, size and shape of your lymphoma.
- Lumbar puncture – (Your doctor will use a needle to take a sample of fluid from near your spine. This is done if your doctor needs to check if your lymphoma is in your brain or spinal cord).
- Bone marrow biopsy – this involves the doctor placing a needle into your lower back and into your hip bone where your blood cells are made. There are two samples the doctor will take during this procedure, including:
Bone marrow aspirate (BMA): this test takes a small amount of the liquid found in the bone marrow space.
Bone marrow aspirate trephine (BMAT): this test takes a small sample of the bone marrow tissue.
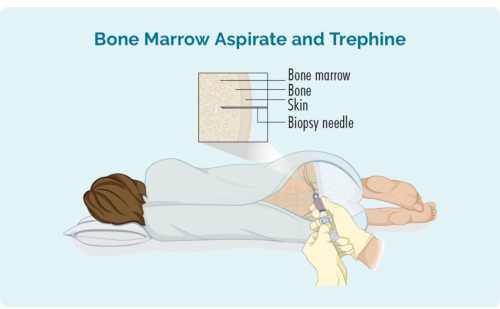
Samples are then sent to pathology where they are checked for signs of lymphoma.
The process for this can differ depending on where you live and where you’re having treatment. However, it will usually include a local anaesthetic to numb the area.
In some hospitals, you may be given light sedation which helps you to relax, and can stop you from remembering the procedure. You may not need this though, and may instead have a “green whistle” to suck on. This green whistle has a pain killing medication in it called Penthrox or methoxyflurane, that you use as needed during the procedure.
Ask your doctor what is available to make you more comfortable during the procedure. If you have any question about their decisions, ask them to explain their reasons.
Your lymphoma cells have a different growth pattern, and look different to normal cells. The grade of your lymphoma is how quickly your lymphoma cells are growing, which affects the way they look under a microscope. The grades are Grades 1-4 (low, intermediate, high). If you have a higher grade lymphoma, your lymphoma cells will look the most different from normal cells, because they are growing too quickly to develop properly. An overview of the grades is below.
- G1 – low grade – your cells look close to normal. They grow and spread slowly.
- G2 – intermediate grade – your cells are starting to look different but some normal cells exist. They grow and spread at a moderate rate.
- G3 – high grade – your cells look fairly different with a few normal cells. They grow and spread faster.
- G4 – high grade – your cells look most different to normal. They grow and spread the fastest.
For more detailed information on diagnosis, staging and grading please see our webpage here.
Understanding Your Marginal Zone Lymphoma (MZL) Cytogenetics
Genetics is very complex, and often an unfamiliar topic to many people. Below we aim to explain some of the genetics you may hear about while learning about your lymphoma. It is not important for you to fully understand and remember everything here. The 4 main things we want you to remember are:
- genetic changes can contribute to the development of lymphoma
- some genetics are present when you are first diagnosed, while others develop later on
- the type of genetic changes you have can change the type of treatment that will best work for you
- ask your doctor if you have any genetic changes that may impact your MZL and treatment
If you would like to learn a little more, please read on, otherwise you can skip to the next section.
Cytogenetics tests will look for changes in your chromosomes or genes. We usually have 23 pairs of chromosomes, and they are numbered according to their size. Your chromosomes may look a little different when you have Marginal Zone Lymphoma (MZL).
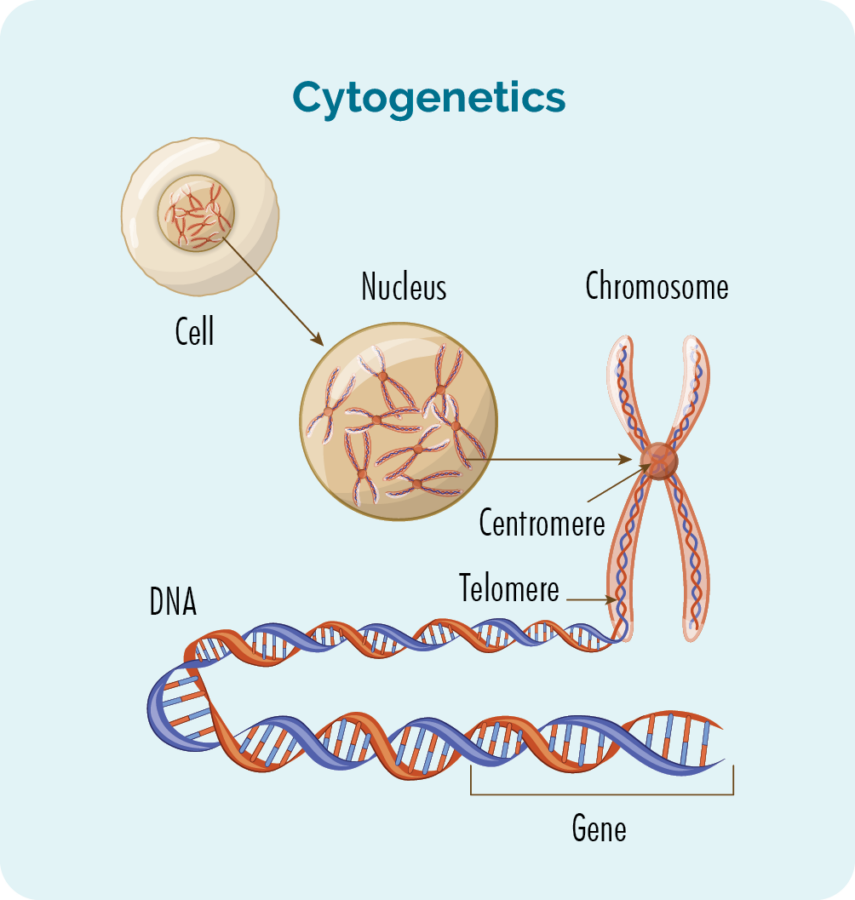
What are genes and chromosomes
- Each cell that makes up our body has a nucleus.
- Inside the nucleus are the 23 pairs of chromosomes.
- Each chromosome is made from long strands of DNA (deoxyribonucleic acid) that contain our genes.
- DNA strands are made from groups of genes.
- Our genes provide the code needed to make all the cells and proteins in our body, and tells them how to look or act.
- A change in your chromosomes or genes may also be called a genetic variation or a mutation.
- Lymphocytes can become lymphoma cells due to genetic changes within the cells.
Your lymphoma biopsy may be looked at by a specialist pathologist to see if you have any gene mutations. If you have a genetic variation, your proteins and cells may not work properly.
What genetic variations happen in Marginal Zone Lymphoma (MZL)?
Translocations
Some mutations that can occur in MZL are called translocations. This is when a piece of two different chromosomes break off and swap places. When it is a piece of the shorter top part of the chromosome that has translocated, it is represented with a (p). If it is from the longer, bottom part it is represented with a (q).
There can also be a number added to this, which refers to the exact location (or gene) on the top or bottom part. For example, a genetic mutation seen in some people with MZL is called t(11:18) (q21:q21).
This means that a section from the bottom, long section (q) of chromosomes 11 and 18, in the 21st segment (a gene), have swapped places.
This translocation is also called an API-2/MALT1 fusion because the gene on the 11th chromosome, at the 21st segment is called API-2, and the gene at the 21st segment of the 18th chromosome is called MALT1.
Other translocations can occur and follow the same naming rationale.
Trisomy
Trisomy is a genetic change that can occur when you have an extra copy of part, or all of one of your chromosomes. These can include an extra copy of your 3rd, 7th, 12th or 18th chromosome. These changes are written as Trisomy 3, Trisomy 7, Trisomy 12 or Trisomy 18.
Deletion
A deletion occurs when a section of one of your chromosomes, including the genes on that section are completely missing. With the gene missing, your body is unable to follow instructions that gene would give – such as telling cancer cells to stop growing.
An example of this is when there is a deletion of the short upper section of your 17th chromosome. This is called a del(17p). Chromosome 17p is where your p53 gene is located. p53 is a tumour suppressor gene.
Tumour Suppressor Genes
Tumour suppressor genes are able to identify when cells are damaged and becoming cancerous. If this happens, they instruct the cell to repair itself, or die – preventing the development of cancers including lymphoma.
If you have a del(17p), the damaged cells don’t get that message to stop growing or repair themselves, so they continue to grow and make more damaged cells, resulting in cancer.
Treatment for Marginal Zone Lymphoma (MZL)
Questions for your doctor before you start treatment
It can be difficult to know what questions to ask when you are starting treatment. If you don’t know, what you don’t, how can you know what to ask?
Having the right information can help you feel more confident and know what to expect. It can also help you plan ahead for what you may need.
We put together a list of questions you may find helpful. Of course, everyone’s situation is unique, so these questions do not cover everything, but they do give a good start.
Click on the link below to download a printable PDF of questions for your doctor.
Planning Treatment
Once all of your tests and scans have been completed, your doctor will review them to choose the best possible treatment for you. At some cancer centers, the doctor will also meet with a team of specialists to discuss the best treatment option. This is called a multidisciplinary team (MDT) meeting.
Your doctor will consider many factors about you and your MZL. Decisions on when, or if you need to start treatment, and what treatment is best are based on:
- The subtype of MZL you have.
- Your individual stage of MZL, genetic changes and symptoms .
- How old you are and your past medical history and general health.
- Your current physical and mental wellbeing.
- Any preferences you have for treatment after being told about your choices.
Other tests you may need
More tests may be ordered before you start treatment to make sure your heart, lungs and kidneys are able to cope with treatment. These may include an ECG (electrocardiogram), lung function test or 24-hour urine collection.
Your doctor or cancer nurse can explain your treatment plan and the possible side-effects to you. They can also answer any question you might have. It is important you ask them questions about anything you don’t understand or are worried about.
Treatment Types
Below we have an overview of the different treatment types. If you would like more detailed information, please see our treatments webpage here.
Treatments options can include any of the following:
Watch and Wait (active monitoring)
Many people with MZL may not need treatment straight away, or at all. Watch and wait is a time where you are actively monitored by your medical team, but do not need treatment. This is a great approach if your disease is stable, and not causing worrying symptoms. MZL can remain stable with little, to no symptoms for many months or years. Your treating team will be actively monitoring you with regular appointments and tests, so they will be able to identify early, if you need to start treatment. This approach is used successfully with many indolent lymphomas.
Supportive Care
Supportive care helps you cope better with your disease, treatments and concerns. It may include:
- providing treatments to manage side effects.
- assisting you with planning your health care needs .
- support to help you live well with your lymphoma.
- helping you access your super or Centrelink entitlements.
- supporting your immune system with medications such as Intragam (antibodies) or vaccines. Not all vaccines are safe or effective when you are having treatment though, so please talk to your treating team before having any vaccines.
Different Health Care Professionals that may provide supportive care
- your local general practitioner (GP)
- social workers
- physiotherapist
- occupational therapists
- psychologist or counselor
- palliative care team
- haematology/oncology treating team.
Depending on where you’re having treatment, there may be different services available. Ask your nurse or doctor about what supportive care is available to you.
Radiation treatment (Radiotherapy)
Radiotherapy uses radiation to kill cancer cells. It is like high-energy X-rays and is performed every day, usually from Monday to Friday for several weeks. It is can be used to cure cancer, to help get you into remission, or to manage some symptoms.
Antibiotics
Some MALT lymphomas can be treated with antibiotics because the lymphoma often stops growing once the infection is treated. This is common in gastric MALT caused by H. pylori infections, or for non-gastric MALTs where the cause is an infection in or around the eyes.
Surgery
Surgery may be used to remove the lymphoma entirely. This may be needed if you have splenic lymphoma to remove your whole spleen. This surgery is called a splenectomy. You may also be offered surgery if you have another subtype of MZL and the lymphoma is in only one small area of your body.
Chemotherapy (chemo)
Chemo can be given as a tablet and/ or be given as a drip (infusion) into your vein (into your bloodstream) at a cancer clinic or hospital. Several different chemo medications may be combined with another treatment. Chemo kills fast growing cancer cells, but can also affect your good cells that grow fast, causing side effects.
Monoclonal Antibody (MAB)
You may have a MAB infusion at a cancer clinic or hospital. MABs attach to the lymphoma cell and attract other disease fighting white blood cells and proteins to the cancer. This helps your own immune system fight the MZL.
Chemo-immunotherapy
Chemotherapy combined with a monoclonal antibody (for example, rituximab).
Targeted therapy
You may take these as a tablet or infusion into your vein. Oral therapies may be taken at home, though some will require a short hospital stay. If you have an infusion, you may have it at a day clinic or in a hospital. Targeted therapies attach to the lymphoma cell and block signals it needs to grow and produce more cells. This stops the cancer from growing, and causes the lymphoma cells to die off.
Stem-cell transplant (SCT) / Bone-marrow transplant
If you have had previous treatment and relapse in a short amount of time, you may be offered a stem-cell transplant (adults and children), or bone marrow transplant (children). However, this will not be a suitable option for everyone. These are complex procedures and you can find more information on them here.
First-Line Treatment
Starting Therapy

You may not need treatment when you’re first diagnosed with MZL. Instead, you may go on watch and wait. This is common for people with stage 1 or 2 disease, and even some people with stage 3 disease if it is stable and not causing you symptoms.
In some cases, you will start treatment. Treatment is likely to be an option for you if you have an advanced stage MZL, are experiencing symptoms or if your disease has started to get worse after being on watch and wait. When you do start treatment for the first time, it is called first-line therapy.
If you know the name of the treatment you will be receiving, you can find more information here.
Gastric MALT Marginal Zone Lymphoma (MZL)
Believe it or not, the standard first-line treatment for Gastric MALT MZL is antibiotics. This is because it is caused by bacteria (H. pylori). By getting rid of the H. pylori, the gastric MALT MZL is also usually is cured. However, H. Pylori is a pretty stubborn bacteria, and can be difficult to get rid of. You will need a combination of antibiotics over several weeks to get rid of the H. Pylori.
You will also likely have another type of medication called a proton pump inhibitor. Examples of proton pump inhibitors include pantoprazole, omeprazole and esomeprazole. These are given to help repair any stomach ulcers or reflux you have from the infection.
It can take a long time, possibly years for the lymphoma to disappear after antibiotic therapy. However, with the infection gone the lymphoma should not grow during that time, and you may not need any further treatment. You will likely go on to watch and wait so your medical team can monitor your progress.
Other treatment options you may be offered
- Watch and Wait (active monitoring)
- Radiation treatment (Radiotherapy)
- Surgery
- Monoclonal Antibody (MAB) – rituximab, with or without chemotherapy
- Chemo-immunotherapy
- Possible clinical trials if eligible – talk to your treating team about what clinical trials are available.
Non-Gastric MALT Marginal Zone Lymphoma (MZL)
- Antibiotics – if lymphoma is around your eyes
- Watch and Wait (active monitoring)
- Surgery – if the lymphoma is only affecting one part of your body such as lung or breast
- Radiation treatment (Radiotherapy)
- Chemotherapy (chemo)
- Monoclonal Antibody (MAB)
- Chemo-immunotherapy
- Possible clinical trials if eligible – talk to your treating team about what clinical trials are available.
Early stage
- Watch and Wait (active monitoring)
- Radiation treatment (Radiotherapy)
- Possible clinical trials if eligible – talk to your treating team about what clinical trials are available
Advanced stage
- Chemotherapy (chemo)
- Monoclonal Antibody (MAB)
- Chemo-immunotherapy
- Possible clinical trials if eligible – talk to your treating team about what clinical trials are available
- Watch and Wait (active monitoring)
- Radiation treatment (Radiotherapy)
- Chemotherapy (chemo)
- Monoclonal Antibody (MAB)
- Chemo-immunotherapy
- Possible clinical trials if eligible – talk to your treating team about what clinical trials are available
Second-Line and Ongoing Treatment

What happens when you relapse?
After treatment you will likely go into remission. Remission is a period of time where you have no signs of MZL left in your body, or when the MZL is under control and doesn’t need treatment. Remission can last for many years, but eventually MZL usually comes back (relapses). Depending on how long you were in remission, you may be offered the same treatment again, or a different treatment.
Refractory Marginal Zone Lymphoma (MZL)
In rare cases, you may not achieve remission with first-line treatment. When this happens, your MZL is called “refractory”. If you have refractory MZL your doctor will offer you a different medication.
Treatment for relapsed or refractory lymphoma is called second-line therapy. The goal of second-line treatment is to put you into remission again.
If you have further remission, then relapse and have more treatment, these next treatments are called third-line therapy, fourth-line therapy and so on.
This pattern may repeat itself over many years.
Click on the headings below to learn what second-line treatments you may be offered.
- Watch and wait
- Antibiotics
- Radiation
- Monoclonal Antibody (MAB)
- Chemotherapy
- Chemoimmunotherapy
- Targeted therapy (such as zanubrutinib if you have previously had CD20+ targeting treatment, such as rituximab or obinutuzumab)
- Possible clinical trials if eligible – talk to your treating team about what clinical trials are available.
- Watch and Wait (active monitoring)
- Chemotherapy (chemo)
- Monoclonal Antibody (MAB)
- Chemo-immunotherapy
- Targeted therapy (such as zanubrutinib if you have previously had CD20+ targeting treatment, such as rituximab or obinutuzumab)
- Stem-cell transplant (SCT)
- Possible clinical trials if eligible – talk to your treating team about what clinical trials are available.
- Watch and Wait (active monitoring)
- Splenectomy – surgery
- Chemotherapy (chemo)
- Monoclonal Antibody (MAB)
- Chemo-immunotherapy
- Targeted therapy (such as zanubrutinib if you have previously had CD20+ targeting treatment, such as rituximab or obinutuzumab)
- Stem-cell transplant (SCT)
- Possible clinical trials if eligible – talk to your treating team about what clinical trials are available.
Side effects of Marginal Zone Lymphoma (MZL) Treatment
There are many different side effects of treatment and they are dependent on what treatment has been given. The treating doctor and/or cancer nurse can explain the specific side effects prior to your treatment.
One of the common side effects of lymphoma and its treatment include low blood counts. The table below provides an overview on these blood cells and symptoms.
White cells | Red Cells | Platelets | |
Medical Name | Neutrophils & Lymphocytes | Erythrocytes | Platelets |
What do they do? | Fight Infection | Carry oxygen | Stop bleeding |
What is a shortage called? | Neutropenia & lymphopenia | Anaemia | Thrombocytopenia |
How will this affect my body? | You will get more infections and may have difficulty getting rid of them even with taking antibiotics. | You may have pale skin, feel tired, breathless, cold and dizzy. | You may bruise easily, or have bleeding that doesn’t stop quickly when you have a cut. |
What will my treating team do to fix this? |
|
|
|
If all your blood cells are low this is called ‘pancytopenia’. You may need to go to hospital for treatment to help improve your blood count levels.
Other common side effects of Marginal Zone Lymphoma (MZL) Treatments
- Feeling sick in the stomach (nausea) and/or vomiting.
- Sore mouth (mucositis). You may also notice a change in the taste of food and drinks.
- Bowel problems such as constipation or diarrhoea.
- Tiredness or a lack of energy not helped by rest or sleep (fatigue).
- Muscle aches and pains (myalgia).
- Joint aches and pains (arthralgia).
- Hair loss and/or thinning (alopecia).
- Mind fogginess and difficulty in remembering things (chemo brain).
- Changed sensation in your hands and feet such as tingling, pins and needles or pain (neuropathy).
- Reduced fertility or early menopause (change of life).
For more information about specific side effects and how you can manage them, click on the button below.
Clinical Trials
There are many treatments options being tested in clinical trials around the world for patients with MZL. We recommend that anytime you need to start new treatments, you ask your doctor about clinical trials you may be eligible for.
Clinical trials are important to find new medicines, or combinations of medicines to improve treatment of MZL in the future.
They can also offer you a chance to try a new medicine, combination of medicines or other treatments that you would not be able to get outside of the trial. If you are interested in participating in a clinical trial, ask your doctor what clinical trials you are eligible for.
For more information on clinical trials, please read our ‘Understanding Clinical Trials’ fact sheet or visit our webpage.
Prognosis and Survivorship - Living with Marginal Zone Lymphoma (MZL)
Prognosis
Prognosis refers to how your MZL is expected to behave, and respond to treatment. Most indolent lymphomas, including MZL develop slowly over a long period of time. They usually respond well to treatment, but are often not curable. However, many people live well without symptoms for long periods of time. There is a good chance you will also live a normal life span.
Your own prognosis is a very individual thing and takes into consideration many factors including your age, overall health, genetics, response to treatments and access to care.
Ask your doctor about your own prognosis and what they expect you will get from your treatments.
Survivorship – Living with cancer
Survivorship refers to people who have been diagnosed with cancer at any point in their lives. It begins at the time you are diagnosed and continues throughout your life. The aim of survivorship in lymphoma, is to ensure you live with the best quality of life.
A healthy lifestyle, or some lifestyle changes after treatment may be a great help to your recovery. There are many things you can do to live well with MZL. We have a range of factsheets with useful information on how to live well with lymphoma. Links to these are at the bottom of this section.
Many people find after a cancer diagnosis or treatment that their goals and priorities in life change. Getting to know what your ‘new normal’ is, can take time and be frustrating. Expectations of your family and friends may be different to yours. You may feel isolated, fatigued or any number of different emotions that can change each day.
Main goals of survivorship
The main goals of survivorship are to help you:
- be as active as possible in your work, family, and other life roles.
- lessen the side effects and symptoms of the cancer and its treatment.
- identify and manage any late side effects.
- help keep you as independent as possible.
- improve your quality of life and maintain good mental health.
Cancer rehabilitation
Different types of cancer rehabilitation may be recommended to you. This could mean any of a wide range of services such as:
- physical therapy for pain management or to improve your movement.
- nutrition and exercise planning.
- emotional, career and financial counselling.
We have some great tips for living well with lymphoma in our factsheets below:
- Fear of cancer recurrence and scan anxiety
- Sleep management and lymphoma
- Exercise and lymphoma
- Fatigue and lymphoma
- Sexuality and intimacy
- Emotional impact of lymphoma diagnosis and treatment
- Emotional impact of living with lymphoma
- Emotional impact of lymphoma after completing lymphoma treatment
- Caring for someone with Lymphoma
- Emotional impact of relapsed or refractory lymphoma
- Complementary and alternative therapies: Lymphoma
- Self-care and Lymphoma
- Nutrition and Lymphoma
Transformed Lymphoma
Transformed Lymphoma is when an indolent – slow growing lymphoma changes and “transforms” into an aggressive – or fast growing lymphoma. This is very rare with MZL, occurring in less than 1 person for every 100,000 people with MZL. If your MZL does transform, you can find more information on transformed lymphoma here.